Abstract
Surrogates’ decisions to withhold or withdraw life-sustaining treatments (LSTs) are pervasive. However, the factors influencing surrogates’ decisions to initiate LSTs are relatively unknown. We present evidence from two experiments indicating that some surrogates’ decisions about when to initiate LSTs can be predictably manipulated. Factors that influence surrogate decisions about LSTs include the patient’s cognitive state, the patient’s age, the percentage of doctors not recommending the initiation of LSTs, the percentage of patients in similar situations not wanting LSTs, and default treatment settings. These results suggest that some people may use heuristics when making these important life-and-death decisions. These findings may have important moral implications for improving surrogate decisions about LSTs and reconsidering paternalism.
Similar content being viewed by others
Introduction
Imagine your spouse is hospitalized after having a heart attack and is unconscious. The doctors ask you what non-standard options you want for your spouse. Among these options are television (TV) on demand, CPR, a breathing machine, an overnight stay, a private room, or a feeding tube. If you love your spouse, which options would you select? Now imagine the same situation except that the doctors ask you which options you do not want to select. Would that mild difference change your selection?
It might. We present evidence from two experiments indicating that some surrogates (people who make decisions for another person) are predictably influenced by factors that suggest they use heuristics (or quick “rules of thumb”) when making decisions about some life-sustaining treatments (LSTs). That surrogates might use heuristics could have important moral implications for improving surrogate decision-making and reconsidering paternalism. In particular, some forms of paternalism for some medical decisions may be not only desirable but also unavoidable (Sunstein and Thaler 2003; Thaler and Sunstein 2008; Trout 2005).
Folk Judgments and Life-Sustaining Treatments
Active euthanasia (i.e., actively killing a patient in order to avoid almost certain future pain when recovery is not likely) has been the focus of many contemporary philosophical arguments about end-of-life decisions (Brock 1992). Seventy-five percent of Americans (Moore 2005), 63 percent of those who have a terminal illness (Wilson, Pinocchio, and McPherson 2007), and even most grade-schoolers think active voluntary euthanasia is sometimes permissible (Pousset et al. 2009). However, the withholding or withdrawal of some LSTs is a practice that dwarfs the number of instances of active euthanasia. The American Medical Association (AMA) defines an LST as “any treatment that serves to prolong life without reversing the underlying medical condition” (2010, 88). According to one study of intensive care units (ICUs) in the United States, nearly 77 percent of all deaths involved withholding or withdrawing LSTs (Prendergast, Claessens, and Luce 1998). Often, decisions about withholding or withdrawing LSTs are made for patients who are unable to decide for themselves (e.g., they are unconscious). Around 50 percent of all nursing home decisions and 75 percent of life-threatening hospital decisions involve incapacitated patients (Rid and Wendler 2010). In one study, for example, in the period of one month, 73 percent of doctors made a medical decision for a patient who could not do so and 81 percent of those decisions involved some form of LSTs (Torke et al. 2009). These considerations suggest that instances of people making decisions about LSTs involving another person are pervasive.
To some degree, legal issues surrounding surrogate decision-making are complex and vary around the world. The American Medical Association (2010) has offered some guidance about surrogate decision-making involving LSTs (see Opinion 2.20). Typically, when a patient is incapacitated, a family member should be designated to be the surrogate decision-maker either through an advance directive or ad hoc at the time a decision-maker is needed. (The former, however, is preferred, although there remains in many societies unawareness of or resistance to the drafting of advance directives.) Doctors should work closely with these surrogates and are tasked with informing them of relevant medical details as well as the surrogate’s role as a decision-maker. This role involves the surrogate using the “substituted judgment” standard where the surrogate is supposed to make treatment decisions the patient would have made if able. In most circumstances, the surrogate’s decision is what should be acted upon. However, in some rare circumstances, the surrogate’s decision could be questioned or even overturned. For example, if there is clear information that the decision goes against what the patient would have decided if the patient were able, this could give cause to overturn a surrogate’s decision. While the surrogate decision-making process may differ in other parts of the world, the policies of the AMA indicate how one country with a large population (i.e., the United States) recommends handling surrogate decisions about LSTs.
But how do surrogates actually go about making decisions about LSTs? This question is straightforwardly empirical.Footnote 1 Unfortunately, many models of how people make decisions about life-sustaining treatments are not informed by empirical research (Teno, Nelson, and Lynn 1994). Generally, we know that many people, even well-educated and highly intelligent people, use a host of heuristics when making decisions in a variety of circumstances (Cokely and Kelley 2009; Gigerenzer, Todd, and the ABC Group 1999). These circumstances can include surrogates’ decisions about medical care. For example, surrogates sometimes have an “over-treatment” bias. That is, surrogates are often biased toward giving significantly more treatment for the patient than the patient would want (Sulmasy, Terry, and Weisman 1998; Uhlmann, Pearlman, and Cain 1988; Ditto, Danks, and Smucker 2001; Fagerlin et al. 2001; Marks and Arkes 2008). If substituted judgment is the standard for surrogate decisions, the over-treatment bias may prevent some people from carrying out the patient’s wishes. Identifying and possibly correcting (or harnessing) these types of biases is therefore important for accurately applying the substituted judgment standard.
As the over-treatment bias indicates, people often have predictable decision-making preferences. These preferences in many instances may indicate that people use heuristics (i.e., fast and frugal decision rules) when making decisions under uncertain conditions that involve cognitive and/or time constraints. Importantly, heuristics are sometimes generalizable to other different but sufficiently similar environments or decision tasks (Gigerenzer, Todd, and the ABC group 1999). This is not to say, however, that the same heuristic can be used in any situation. For example, those who may be biased with regard to over-treatment may use what could be called the “if sick then treat” heuristic. Since heuristics can sometimes generalize to new situations, the “if sick then treat” heuristic may not only be used in medical decisions in hospitals, it may also be used for some similar decisions at home about children or pets. However, the “if sick then treat” heuristic might not be used in determining how to service one’s car.
Along these lines, we will focus on some heuristics that are likely involved in surrogate decisions about LSTs. People sometimes use the “follow the leader” heuristic. That is, one fast and frugal rule is just to do what a leader or authority figure is doing. For example, there is some evidence that people sometimes make financial decisions and investments based on what they think an expert, or somebody who is more competent, suggests or does (Gehrig et al. 2008). People also tend to “follow the herd” or agree with what those around them are thinking or doing (e.g., Martin, Gardkikiotis, and Hewston 2002; Gerard, Wilhelmy, and Conolley 1968; Lascu, Bearden, and Rose 1995; Nordholm 1975; Goldberg 1954; Deutsch and Gerard 1955). For example, Martin, Gardkikiotis, and Hewston (2002) showed that participants’ perception of the percentage of people who thought that voluntary active euthanasia should be legalized influenced their opinion about the legalization of voluntary active euthanasia. When more than 50 percent of the population (e.g., 82 percent or 52 percent) was described as supporting voluntary active euthanasia, people tended to agree more that voluntary active euthanasia should be legal compared to groups who received information that a minority (e.g., 18 percent or 48 percent) supported voluntary active euthanasia. So, these studies suggest that people have a bias (i.e., have a preference) to follow what those around them are doing or thinking.
There is also tendency among people to prefer providing some medical treatments for individuals who are younger compared to those who are older. It is a fact that older patients generally receive fewer procedures and less expensive hospital care than younger patients in similar situations. In a study of 9,105 patients who at some point could have used some LST (including ventilator support, major surgery, or dialysis), those who were younger than 70 tended to get those LSTs at a higher rate than those who were older than 70 (Hammel, Teno, and Goldman 1999). This effect persisted even after preferences for care and prognoses were controlled for. Hence, these data suggest that people are systematically biased to prefer treatment of the young and not the old.
Finally, default settings can have a major impact on some decisions. In a famous example, the default settings for organ donation can have a remarkable impact on the number of people who actually decide to be possible organ donors (Sunstein and Thaler 2003). In many Western European countries, people are defaulted into being organ donors. That is, they are free not to be organ donors but they must take some (trivial) step not to be on organ donor (e.g., checking a box). In these countries, around 90 percent of people are possible organ donors. However, in the United States, the default is different. People are defaulted into not being an organ donor and have to take some (trivial) step to become an organ donor. This modest change in environment has resulted in approximately 28 percent of Americans being possible organ donors. This suggests that people often use the “status quo” or “defaults” heuristic (Todd and Gigerenzer 2007).
Because heuristics can generalize to similar yet different judgment tasks, it is likely that some people use some of these heuristics to make decisions about initiating some LSTs. Allen-Burge and Haley (1997) conducted a study suggesting that surrogates use heuristics when making decisions about some LSTs. One of their main goals was to determine the effect of some age-related cognitive impairments (i.e., dementia) on people’s willingness to initiate LSTs for hypothetical family members. To show that impaired cognitive states sometimes play a role in surrogates’ decisions to initiate LSTs, they gave participants a description of a hypothetical family member who is in the hospital because of a recent heart attack. While in the hospital, the family member has another heart attack and is unconscious. In one scenario, the family member is described in a way that indicates he has a mild form of dementia (e.g., he gets lost inside the house, he has had problems with his memory), whereas the other scenario does not have this information. This modification in condition resulted in differences in preferences for initiating three types of LSTs: CPR, CPR and breathing machine, and CPR and feeding tube. Hence, these data suggest that some people are systematically biased by the cognitive states of patients. People are less likely to initiate some LSTs for individuals with some kinds of cognitive impairment compared to those without.
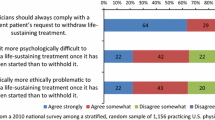
But relatively little is actually known about how people actually make decisions about LSTs and what heuristics might be involved. A recent meta-analysis (Shalowitz, Garrett-Mayer, and Wendler 2006) found 16 studies that dealt with surrogate decision-making, and only some of those dealt with surrogates’ decisions about LSTs. There has been a fair amount of research about the wishes of competent individuals concerning LSTs (Sharman et al. 2008; Wilson, Pinocchio, and McPherson 2007), how doctors react to decisions involving LSTs (Torke, Sachs, and Helft 2011), and how accurate some surrogates are about determining LSTs (Shalowitz, Garrett-Mayer, and Wendler 2006; Marks and Arkes 2008). However, we do not know much about what factors are actually involved in surrogates’ decisions about LSTs. We aimed to help to begin to fill this lacuna.
Experiment 1a
The aim of Experiment 1a was to replicate and extend a study by Allen-Burge and Haley (1997) indicating that the cognitive state of the patient influenced a surrogate’s decisions about initiating LSTs. We wanted to control for several problematic confounds in their scenarios: For example, the person without dementia is an active gardener, helps others with household repairs, and travels frequently with his wife in their recreational vehicle, whereas the person with dementia is not described in these ways (see also Williams et al. 2007). Any one of these differences could plausibly be responsible for the observed differences instead of the illness itself. By removing these possible confounds, we can better isolate the effect of the cognitive state of the individual on preferences about some LSTs. We predicted that, even after removing the confounds, people would prefer LSTs for a person who is described as not having dementia compared to one who does (Allen-Burge and Haley 1997; Hammel, Teno, and Goldman 1999).
Participants
All of our experiments received institutional review board (IRB) approval for the use of human subjects. Before being allowed to take the survey, participants completed an informed consent form. One hundred and one participants were recruited online from Amazon’s Mechanical Turk—a service that gathers a group of individuals who express an interest in taking surveys (i.e., an online panel) for a cash award. This procedure is generally acknowledged to be as good as if not better than using other convenience samples (e.g., college undergraduate students) (Buhrmester, Kwang, and Gosling 2011). These participants were screened to ensure that they resided in the United States and were over the age of 18. Participants came from diverse educational backgrounds: having completed a high school diploma (12 percent), a bachelor’s degree or at least some college (72 percent), or a graduate degree (16 percent). Political affiliation was also diverse: 45 percent reported they were Democrats, 19 percent Republicans, 26 percent “other,” and 10 percent chose not to indicate affiliation. We offered 0.15–0.25 USD per survey depending on factors such as the length of the survey.Footnote 2 Eight participants were excluded for failing a basic comprehension question (see below). The mean age was 31.63 (SD = 11.40), ranging from 18 to 69. There were 29 males (31 percent) and 63 females (68 percent) and one participant who did not indicate sex (1 percent).
The Case: Dementia vs. No Dementia
Participants were randomly assigned to read only one of two scenarios based on those used by Allen-Burge and Haley (1997). One scenario depicted a man with dementia (indicated by the areas in the case below that are underlined) and the other without dementia.
David Johnson is a 74-year-old retired electrician who was recently hospitalized after suffering cardiac arrest. He has been treated for hypertension. He was complaining of mild chest pain for two weeks prior to the hospitalization. Mr. Johnson lives with his wife of 55 years in their own home. David and his wife enjoyed traveling in their recreational vehicle (RV). When at home, he liked to do volunteer work, garden, and sing in his church choir. Before this hospitalization, Mr. Johnson was rarely sick or in pain. However, about eight years ago, he began having problems with his memory. He is now almost totally dependent on his wife for such things as dressing and cooking. He has children and siblings who live near him and several close friends who see him often. Others consider the Johnson’s a close family, and David and his wife are financially secure.
Participants then rated their level of agreement with the following questions on a five-point Likert scale (1 = strongly disagree, 2 = disagree, 3 = neither disagree nor agree, 4 = agree, 5 = strongly agree):
-
1.
Suppose David experiences another heart attack while in the hospital and his heart stops. In this case, if you were a member of David’s family, how likely would you be to agree that the medical staff should perform cardiopulmonary resuscitation (CPR)?
-
2.
Suppose David experiences another heart attack while in the hospital, his heart stops, and he is unable to breathe on his own. In this case, if you were a member of David’s family, how likely would you be to agree that the medical staff should perform CPR and place David on a ventilator (breathing machine) for an indefinite period of time?
-
3.
Suppose David experiences another heart attack while in the hospital, his heart stops, and he is unable to swallow food. In this case, if you were a member of David’s family, how likely would you be to agree that the medical staff should perform CPR and place David on a feeding tube for an indefinite period of time?
Following these questions, participants answered a comprehension question: “Why is David in the hospital?” Participants could not return to the scenarios once they were asked the comprehension question.
Results and Discussion
Overall, a multivariate analysis of variance (MANOVA) revealed a moderately sized effect in the predicted direction F (3, 89) = 3.39, p = .02, η 2p = .10. To further determine whether every judgment differed as a function of condition, an analysis of variance (ANOVA) was conducted on each dependent variable (i.e., answers to questions 1–3) with cognitive state as the independent variable.Footnote 3 There were statistically significant differences with each dependent variable: CPR F (1, 91) = 8.44, p = .005, η 2p = .09; Breathing Machine F (1, 91) = 5.32, p = .02, η 2p = .06; Feeding Tube F (1, 91) = 5.74, p = .02, η 2p = .06. Means and standard deviations are reported in Table 1.
Even after removing possible confounds, we found the same general pattern of results Allen-Burge and Haley (1997) found—namely, that people had a preference, or bias, for not treating people with dementia compared to people without dementia. Hence, we can have a greater degree of confidence that many people actually have this bias because this result has been replicated without the possible confounds. Since this result suggests that there is something stable about people’s judgments and preferences about cases involving LSTs, these scenarios formed the basis of the scenarios in Experiments 1b–1d.
Experiment 1b
Doctors are authority figures when it comes to medical decisions and are often involved in surrogate decisions about LSTs (Torke et al. 2009). Although doctors may not hold the legal authority to make final decisions when a surrogate is appointed, their suggestions as authority figures can have a great impact on the decision-maker. Indeed, according the American Medical Association, it is one of the doctor’s duties to inform the surrogate about medical options as well as the surrogate’s role in the decision-making process. Because of doctors’ position of authority or expertise, surrogates’ knowledge of doctor recommendations might trigger the “follow the leader (or expert)” heuristic resulting in more surrogate decisions in the direction of the majority of doctors’ recommendations (Sadrieh, Güth, and Hammerstein 2002). We predicted that when a greater percentage of doctors did not think initiating LSTs was the best treatment option, more surrogates would decide not to initiate LSTs compared to when a minority of doctors thought not initiating LSTs is the right treatment option.
Participants
There were 146 participants. Two underage participants along with 10 who failed a basic comprehension question were excluded. The mean age was 30.20 (SD = 11.12), ranging from 18 to 71. There were 58 males (43 percent) and 76 females (57 percent).
The Case: Doctor Majority vs. Doctor Minority
Participants received the “No Dementia” case as described in Experiment 1a and answered three slightly modified questions. Each question was the same as in Experiment 1a with the exception that information about the percentage of doctors who thought that not initiating the treatment was the best option was added. Only one of the following clauses was added to the last sentence of each question: “if 75 percent (25 percent) of the doctors agree that not initiating treatment is the best option?” For example, the first question for participants in the doctor majority condition was: “Suppose David experiences another heart attack while in the hospital and his heart stops. In this case, if you were a member of David’s family, how likely would you be to agree that the medical staff should perform cardiopulmonary resuscitation (CPR) if 75 percent of the doctors agree that not initiating treatment is the best option?”
Results and Discussion
A MANOVA revealed an overall moderately sized difference in conditions, F (3, 130) = 3.5, p = .02, η 2p = .09. To test whether each dependent variable differed, we performed ANOVAs on all three dependent variables with doctor majority and doctor minority (75 percent v. 25 percent) conditions as independent variables. There were significant differences with responses to Breathing Machine and Feeding Tube and a trend toward significance for CPR: CPR F (1,134) = 2.36, p = .13, η 2p = .02; Breathing Machine F (1, 134) = 10.75, p = .001, η 2p = .07; Feeding Tube F (1, 134) = 6.35, p = .01, η 2p = .05. Treating the “No Dementia” case in Experiment 1a as a control, a MANOVA revealed a moderately strong difference between “No Dementia” and “Doctor Majority,” F (3, 110) = 8.41, p < .001, η 2p = .19. Subsequent ANOVAs revealed differences with each of the dependent variables: CPR F (1, 112) = 24.00, p < .001, η 2p = .18, Breathing Machine F (1, 112) = 8.23, p = .005, η 2p = .07, Feeding Tube F (1, 112) = 10.24, p = .002, η 2p = .08. A MANOVA indicated that there was also an overall effect between “Doctor Minority” and “No Dementia,” F (3, 114) = 6.13, p = .001, η 2p = .14. However, ANOVAs revealed that the only statistically significant difference among the three dependent variables occurred with CPR, F (1, 116) = 11.04, p = .001, η 2p = .09, all other F’s < 1 (See also Table 2).
These data suggest that information about what experts or leaders recommend influenced surrogates’ decisions. When the majority of doctors are inclined not to recommend initiating LSTs, people were much more likely to decide not to initiate LSTs compared to when only the minority made that recommendation. Moreover, there were differences between Doctor Majority and No Dementia. Those who were not provided any information about doctors’ preferences were more likely to want to initiate LSTs compared to those who were informed that a majority of doctors did not recommend initiating LSTs. This may suggest that, in the absence of additional information, participants think that by default doctors recommend treatment (see also Experiment 1c and Experiment 2).Footnote 4
Experiment 1c
People have a tendency to make decisions in accordance with their beliefs about what others around them are deciding (e.g., Martin, Gardikiotis, and Hewstone 2002; Gerard, Wilhelmy, and Conolley 1968; Lascu, Bearden, and Rose 1995; Nordholm 1975; Goldberg 1954). Because some people compare their decisions and attempt to conform to those around them (Martin, Gardikiotis, and Hewstone 2002; Deutsch and Gerard 1955), we predicted that the percentage of patients in similar circumstances who wanted LSTs would influence surrogate decisions to initiate LSTs in that direction (e.g., they use the “follow the herd” heuristic).
Participants
One hundred and nine people participated. Three participants who failed to complete the survey, one underage participant, and eight participants who failed a basic comprehension question were excluded. Thirty-six (37 percent) were male and 61 (63 percent) were female. Ages ranged from 18 to 81 (M = 34.95, SD = 13.95).
The Case: Peer Minority vs. Peer Majority
Participants received the exact same materials as in Experiment 1b, except that the additional clauses were replaced with the corresponding version of the following clauses: “if 75 percent (25 percent) of the people who are David’s age, sex, and race do not want CPR / CPR and a breathing machine / CPR and a feeding tube in this situation?”
Results and Discussion
Overall, a MANOVA revealed moderately sized differences between the “Peer Minority” and “Peer Majority” conditions, F (3, 93) = 3.01, p = .03, η 2p = .09. ANOVAs found predicted differences with each of the dependent variables: CPR F (1, 95) = 6.88, p = .01, η 2p = .07, Breathing Machine F (1, 95) = 3.80, p = .05, η 2p = .04, Feeding Tube F (1, 95) = 4.90, p = .03, η 2p = .05. Means and standard deviations are reported in Table 3. Comparisons with the “No Dementia” case revealed an overall difference with “Peer Majority”: F (3, 95) = 7.47, p < .001, η 2p = .19. ANOVAs revealed differences between CPR F (1, 97) = 17.73, p < .001, η 2p = .16, Feeding Tube F (1, 97) = 6.81, p = .01, η 2p = .07, but not with Breathing Machine F (1, 97) = 2.05, p = .16, η 2p = .02. No reliable differences were found between “No Dementia” and “Peer Minority” (p > .18).
Consistent with and extending previous research, people tended to make decisions congruent with the preferences of those who are like the person for whom the surrogate is making decisions. When compared against a scenario that lacks this information (“No Dementia” from Experiment 1a), there were significant differences when the majority did not want LSTs but no differences when the minority did not want treatment. This might indicate, much like in Experiment 1b, that most people assume that people want treatment unless there are some cues that bring non-treatment to attention.
Experiment 1d
Elder patients with serious illnesses generally receive fewer procedures and less expensive hospital care than younger patients in similar situations. This preferential allocation of hospital services to younger patients is generally not driven by differences in patients’ preferences for LSTs or illness characteristics (Hammel, Teno, and Goldman 1999). Perhaps these differences result from the tendency of physicians to believe erroneously that the majority of older patients do not want LSTs compared to younger patients (Hammel, Teno, and Goldman 1999). Experiment 1d tested whether the tendency of preferring LSTs for younger patients was also found in surrogate decision-making.
Participants
One hundred and fourteen people participated. Fifteen were excluded for failing a basic comprehension question or not completing the survey. The mean age was 31.01 (SD = 9.56), ranging from 18 to 60. There were 52 males (53 percent) and 44 females (44 percent). Three did not report sex or age (3 percent).
The Case: Baby vs. Elder
Participants received one of two scenarios, “Baby” or “Elder”:
David is a 4-day-old baby (74-year-old man). While at home, David had a heart attack. As a result of the heart attack, David suffered brain damage due to lack of oxygen to the brain. David is now in the hospital being treated for the heart attack and brain damage.
After receiving one of these scenarios, participants were asked the same three questions used in Experiment 1a.
Results and Discussion
Overall, a MANOVA found the predicted difference, F (3, 184) = 2.63, p = .05, η 2p = .04. To test differences for each individual variable, ANOVAs were conducted with age as independent variables and answers to the three questions as dependent variables. All differences were statistically significant except for Feeding Tube: CPR F (1, 186) = 6.50, p = .01, η 2p = .03; Breathing Machine F (1, 186) = 8.85, p = .001 η 2p = .03; Feeding Tube F (1, 186) = 2.15, p = .15 η 2p = .01 (See also Table 4).
These data indicate that there is an age bias in surrogate decision-making about some LSTs. It may be that age is not what influences surrogates’ decisions. After all, some LSTs for older patients could be perceived as futile or less effective because of the relatively shorter life expectancy of older versus younger patients. While this may be true, the only difference in information presented in the scenario was the differences in age, and this factor appeared to bias people’s decisions. As such, at a minimum, age appeared to be the cue that may have triggered other information to be recalled (such as quality of life). And if that is the case, then age is a sufficient (although perhaps not necessary) factor that alters some surrogates’ decisions about some LSTs.
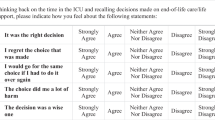
Experiment 2
People sometimes have a tendency to stay with default selections even when it is very easy to choose a different option (e.g., checking a box). Default settings are known to have large impacts on some people’s decisions, for example in organ donation or retirement savings (Johnson and Goldstein 2003; Sunstein and Thaler 2003). Along these lines, participants in Experiment 2 had to choose to opt in or out of the three LSTs along with other “dummy” options. We predicted that surrogates who must opt into an LST would be less likely to initiate LSTs than surrogates who must opt out of initiating LSTs.
Participants
Two hundred and thirty people participated. The mean age was 31.59 (SD = 10.86), ranging from 18 to 59. There were 114 males (50 percent) and 116 females (50 percent).
The Case: Opt In vs. Opt Out
Participants were randomly given only one of two scenarios. One scenario asked the participants to mark which options they would like to have (“Opt In”). The other scenario asked participants to mark which options they do not want to have (“Opt Out”).
Suppose David experiences another heart attack while in the hospital and his heart stops. Imagine you are part of David’s family responsible for making David’s medical decisions. Items 1–10 below are (not) standard care at his hospital, and David will (not) receive any of them if he needs them. However, you can opt out (in) to any of items 1–10 below. Please check all those items you wish to opt out of (in to).
The options participants could (de)select were (presented randomly): TV on demand in room, 24-hour visiting hours, CPR, put him on a breathing machine, physical therapy, overnight stay in hospital, adjustable bed, private room, insert feeding tube, and private nurse. The inclusion of non-medical options was intended to help mask from participants which options were the targets of the experiment.
Results and Discussion
Small effects were found for CPR C2 (N = 230) = 4.60, p = .03, d = .29, and Feeding Tube C2 (N = 230) = 5.84, p = .02, d = .32, while a large effect was found for Breathing Machine C2 (N = 230) = 33.90, p < .001, d = .83. See Table 5.
These results demonstrate another area where defaults impact judgments. Just as in previous studies, people tended to make default congruent decisions. In the present context, participants were asked whether they wanted to opt into some treatment options or not opt out of some treatment options. The mild change in the way the choice was worded altered people’s judgments about seemingly logically identical decisions about some LSTs (see McKenzie, Liersch, and Finkelstein (2006) for an argument that defaults are tacit recommendations, hence the two choices are not logically identical). This is the first demonstration that we know of where defaults affect some surrogate decisions about LSTs. As such, these results are consistent with the people using the “defaults” heuristic.
General Discussion
In our experiments, participants were asked to imagine making decisions to initiate LSTs for a loved one who was incapacitated. Experiment 1 suggested that the following factors influenced surrogates’ judgments: (a) the recent cognitive state of the patient, (b) the percentage of doctors’ recommendations, (c) the percentage of patients in similar situations wanting treatment, and (d) the age of the patient. Experiment 2 suggested that default treatment settings played an important role in surrogates’ decisions to initiate LSTs. These results suggest that many people use some heuristics when making decisions about some LSTs.
These results are important because they may help contribute to some desired outcomes concerning surrogate decisions about LSTs. One of these outcomes is that that we can improve surrogate decision-making by harnessing these biases (Trout 2005). On many accounts, success in surrogate decision-making involves the surrogate making decisions the patient would have made if the patient were able—the substituted judgment standard (see Kuczweski (1999) and the American Medical Association (2010)). But there are several problems with actually employing the substituted judgment standard. One important problem is that surrogates are just not very good at correctly determining patient treatment preferences. One meta-analysis of the accuracy of surrogate decision-making indicated that surrogates were accurate only about 68 percent of the time (Shalowitz, Garrett-Mayer, and Wendler 2006). This success rate is hardly above chance (guessing would be correct 50 percent of the time). And perhaps disturbingly, there is little to no evidence that being a close relative or discussing end-of-life care increases surrogate accuracy (Shalowitz, Garrett-Mayer, and Wendler 2006; Sharman et al. 2008).
Improving accuracy of surrogate decision-making about LSTs in terms of the substituted judgment standard might be achieved simply by providing advance directives where patients indicate their treatment preferences. For example, some may think that close contact with physicians or with family members and long discussions about one’s own treatment preferences might improve accuracy of surrogate decisions (Braun and McCullough 2011). But emerging evidence casts doubt on this simple and direct solution. Advance directives may be inaccurate because people tend to change their minds about end-of-life care, forget that they have changed their minds, and then fail to update their directives with their new preferences (Sharman et al. 2008). Even if we assume that advance directives perfectly match current patient treatment preferences, they still may be of limited use. A surrogate’s reading of an advance directive does not increase surrogates’ accuracy (Sharman et al. 2008), perhaps in part because surrogates tend to make decisions that reduce their responsibility (Rid and Wendler 2010). And physicians are reluctant to override family wishes even if there is an advance directive in place (Teno, Nelson, and Lynn 1994).
But given that people display certain biases, it is possible that we could actually improve surrogate decisions in terms of the substituted judgment standard based on advance directives. For example, imagine that John has an advance directive that indicates that he does not want any LSTs. Given our data, there are a number of steps one could take that would make it more likely that John’s surrogate would decide not to initiate LSTs. For example, we might emphasize some problems with John’s cognitive state. We could explain that many doctors do not recommend initiating LSTs or that many individuals in John’s situation do not want LSTs. We could emphasize that John is elderly. Or, we could simply set the default that John will not receive any LSTs unless action is taken by the surrogate to initiate those LSTs. In all of these ways, we make it less likely that the surrogate would choose to initiate LSTs and thereby increase the chances that the surrogate would make an accurate decision. And, of course, if John does want LSTs, then we could make the corresponding changes to help increase the chances that the surrogate makes the right choice in that situation. Indeed, if we could improve decision-making in these ways, it actually reinforces the need and importance of filling out and respecting advance directives.
While many think that in general biased minds can make better decisions, it is also widely recognized that biased minds can sometimes lead to mistakes (Gigerenzer 2000).Footnote 5 So, in some instances, it may be desirable to de-bias individuals’ decisions about LSTs. Consider again the over-treatment bias where surrogates typically want more treatment for an individual than the individual wants. In these cases, it seems likely that the over-treatment bias will get things wrong by over-treating patients. Our data suggests possible ways to de-bias people and make them less likely to over-treat. For example, take Experiment 1. When some cues are provided (e.g., mental states, doctors’ recommendations, other patients’ preferences, age), we can make it less likely that people would want to initiate treatment. When these cues are absent, most people tend to decide to initiate all three LSTs (consistent with the over-treatment bias). So, by presenting people with this information may be one way to eliminate or reduce these biases.
Increasing accuracy is not the only way that harnessing these types of biases could make decisions better in some sense. Our results could help with other factors such as welfare or social desirability (Halpern, Ubel, and Asch 2007). Many people who do not want to initiate LSTs cite pain or burden on the family as major considerations (Wilson, Pinocchio, and McPherson 2007). In some instances, not initiating LSTs would likely result in an overall better state of affairs because of the absence of unnecessary patient and family suffering. But there are other possible benefits of decreased use of LSTs. The initiation of more LSTs could have socially undesirable effects such as nurse burn-out or suboptimal allocation of resources (Braun and McCullough 2011), leading to overall worse care for patients. If initiating LSTs leads to worse overall welfare or worse overall patient care, then it seems one should take some steps to prevent some LSTs. Our results suggest some possible ways to increase some possibly socially desirable decisions in the same ways that we could improve the accuracy of surrogates’ decisions about some LSTs.
These considerations may indicate that the existence of biases and the use of heuristics naturally justify some kinds of paternalism. This may be true. But we want to emphasize that paternalism concerning LSTs might be justified. The extent, type, and direction of any paternalistic intervention are still unclear. Just because people may be systematically biased does not entail that paternalism is justified even on paternalistic grounds (e.g., increasing welfare) (Berg and Gigerenzer 2007). There may be unknown risks by engaging in a paternalistic policy (Glaeser 2006; Berg and Gigerenzer 2007; Korobkin 2009). For example, we may want to limit risk-taking in certain domains (e.g., alcohol, sex, drugs), so we enact a paternalistic policy that penalizes those who would engage in those behaviors. Typically, penalizing a behavior discourages people from engaging in that behavior. But, in some domains, taking paternalistic measures to penalize risky behaviors actually leads people to engage in even riskier behaviors, leading to unanticipated, worse outcomes (Berg and Gigerenzer 2007). Similarly, there may be some unknowns and unwanted risks associated with enacting paternalistic policies concerning surrogate decisions about LSTs.
These considerations indicate that paternalistic policies are justified, if they are justified, only after a detailed study. The type of study would address the particular costs and benefits associated with a particular paternalistic policy targeting some group of people about a particular issue in a specific environment (cf., Jansen and Wall 2009). And these detailed studies are likely to be complicated and nuanced. For example, we know that not all people (e.g., more intelligent, more experienced) are biased in the same ways or by the same factors (see Rachlinski 2006; Cokely, Kelley, and Gilchrist 2006). As a result, there is not likely to be a one-size-fits-all approach to paternalism, since there will be predictable, stable individual differences in people’s decision processes (Korobkin 2009). Indeed, any model that does not take into account these individual differences runs the risk of being inaccurate (see Cokely and Feltz 2010; Feltz and Cokely in press). Because of these complexities, it is difficult, if not impossible, to recommend any particular policy. To the extent that one can offer any recommendations based on a few studies, the current set of data recommends at most “local” paternalism about LSTs rather than “global” or context-free approaches to paternalism about LSTs (Berg and Gigerenzer 2007; Menard 2010).
Knowing whether and to what extent we should have paternalistic policies about LSTs is uncertain. But understanding whether we should have paternalistic policies toward LSTs is pressing not only because such policies are about high-stakes activities but also because in some instances some forms of paternalism concerning LSTs are likely unavoidable (Sunstein and Thaler 2003). In some situations, we cannot but influence people’s choices by the way the choices are presented (Trout 2005; Sunstein and Thaler 2003; Thaler and Sunstein 2008; Korobkin 2009; Halpern, Ubel, and Asch 2007). Take, for example, the results from Experiment 2. There are only two ways to present choices about LSTs to individuals: either (a) patients are defaulted into LSTs or (b) patients are not defaulted into LSTs. These default settings influenced surrogates’ decisions whether to initiate LSTs. Since there are only two ways to present the question, we must set defaults one way or another—there is no way to present the choice without having some default in place. Because we know these facts, we have no choice but to influence some decisions about LSTs (either by commission or omission). If we have no choice about influencing some decisions about LSTs and we know this, we should simply choose the default that has the highest expected utility (Sunstein and Thaler 2003; Thaler and Sunstein 2008). And by doing that, one enacts a (possibly weak) paternalistic policy.
Notes
Many theorists (e.g., experimental philosophers) have been using empirical methods to help shed light on philosophically important issues. These issues have included ethics (e.g., Nadelhoffer and Feltz 2008), epistemology (e.g., Feltz and Zarpentine 2010; Weinberg, Nichols, and Stich 2001), philosophy of mind (e.g., Cokely and Feltz 2009; Feltz, Cokely, and Nadelhoffer 2009), and applied ethics (Feltz and Cokely in press; Cokely and Feltz in press; Allhoff 2003, 2005).
All of our studies followed this same procedure and the participants had the same basic demographics. Since these demographics were not involved in predictions in our studies, we do not report them in subsequent studies.
One worry with Experiment 1b and 1c is that the prompts indicate doctors’ recommendations against and other patients’ preference against treatment. This may make the prompts particularly difficult to understand. While failures on the comprehension question were consistent with the other studies in Experiment 1, it still could be that many people did not truly understand the nature of the question. If that is the case, then we actually underestimate the effects, since the confusion would reduce the true effect.
For example, because people have a tendency to stick with defaults, that bias may lead to better decisions for things such as organ donation (Johnson and Goldstein 2003). However, these biases can also lead to worse decisions, such as sticking with some default retirement plans that have lower overall expected value (Choi et al. 2002).
References
Allen-Burge, R., and W.E. Haley. 1997. Individual differences and surrogate medical decisions: Differing preferences for life-sustaining treatments. Aging & Mental Health 1(2): 121–131.
Allhoff, F. 2003. Terrorism and torture. International Journal of Applied Philosophy 17(1): 105–118.
Allhoff, F. 2005. A defense of torture: Separation of cases, ticking time-bombs, and moral justification. International Journal of Applied Philosophy 19(2): 243–264.
American Medical Association. 2010. Code of medical ethics. Chicago: American Medical Association.
Berg, N., and G. Gigerenzer. 2007. Psychology implies paternalism? Bounded rationality may reduce the rationale to regulate risk-taking. Social Choice and Welfare 28(2): 337–359.
Braun, U.K., and L.B. McCullough. 2011. Preventing life-sustaining treatment by default. Annals of Family Medicine 9(3): 250–256.
Brock, D.W. 1992. Voluntary active euthanasia. The Hastings Center Report 22(2): 10–22.
Buhrmester, M., T. Kwang, and S.D. Gosling. 2011. Amazon’s Mechanical Turk: A new source of inexpensive, yet high-quality, data? Perspectives on Psychological Science 6(1): 3–5.
Choi, J.J., D. Laibson, B.C. Madrain, and A. Metrick. 2002. Defined contribution pensions: Plan rules, participants decisions, and the path of least resistance. In Tax and the economy, ed. J. Poterba, 67–113. Cambridge, MA: The MIT Press.
Cokely, E.T., and A. Feltz. 2009. Individual differences, judgment biases, and theory-of-mind: Deconstructing the intentional action side effect asymmetry. Journal of Research in Personality 43(1): 18–24.
Cokely, E.T., and A. Feltz. 2010. Adaptive diversity and misbelief. Behavioral and Brain Sciences 32(6): 516.
Cokely, E.T., and A. Feltz. In press. Virtue in business: Morally better, praiseworthy, trustworthy, and more satisfying. Journal of Organizational Moral Psychology.
Cokely, E.T., and C.M. Kelley. 2009. Cognitive abilities and superior decision making under risk: A protocol analysis and process model evaluation. Judgment and Decision Making 4(1): 20–33.
Cokely, E.T., C.M. Kelley, and A.L. Gilchrist. 2006. Sources of individual differences in working memory: Contributions of strategy to capacity. Psychonomic Bulletin and Review 13(6): 991–997.
Deutsch, M., and H.B. Gerard. 1955. A study of normative and informational social influences upon individual judgment. Journal of Abnormal and Social Psychology 51(3): 629–636.
Ditto, P.H., J.H. Danks, W.D. Smucker, et al. 2001. Advance directives as acts of communication: A randomized controlled trial. Archives of Internal Medicine 161(3): 421–430.
Fagerlin, A., P.H. Ditto, J.H. Danks, R.M. Houts, and W.D. Smucker. 2001. Projection in surrogate decisions about life-sustaining medical treatments. Health Psychology 20(3): 166–175.
Feltz, A., and E.T. Cokely. In press. The philosophical personality argument. Philosophical Studies.
Feltz, A., E.T. Cokely, and T. Nadelhoffer. 2009. Natural compatibilism versus natural incompatibilism: Back to the drawing board. Mind & Language 24(1): 1–23.
Feltz, A., and C. Zarpentine. 2010. Do you know more when it matters less? Philosophical Psychology 23(5): 683–706.
Gehrig, T., W. Güth, R. Levínský, and V. Popova. 2008. Do investors optimize, follow heuristics, or listen to experts? Jena Economic Research Papers 86(2): 1–43.
Gerard, H., R. Wilhelmy, and E. Conolley. 1968. Conformity and group size. Journal of Personality and Social Psychology 8: 79–82.
Gigerenzer, G. 2000. Adaptive thinking: Rationality in the real world. New York: Oxford University Press.
Gigerenzer, G., P. Todd, and The ABC Group. 1999. Simple heuristics that make us smart. Oxford: Oxford University Press.
Glaeser, E.L. 2006. Paternalism and psychology. The University of Chicago Law Review 73: 133–156.
Goldberg, S.C. 1954. The situational determinants of conformity to social norms. The Journal of Abnormal and Social Psychology 49(3): 325–329.
Halpern, S.D., P.A. Ubel, and D.A. Asch. 2007. Harnessing the power of default options to improve health care. The New England Journal of Medicine 357(13): 1340–1344.
Hammel, M.B., J.M. Teno, L. Goldman, et al. 1999. Patient age and decisions to withhold life-sustaining treatments from seriously ill, hospitalized adults. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. Annals of Internal Medicine 130(2): 116–125.
Hummel, T.J., and J.R. Sligo. 1971. Empirical comparison of univariate and multivariate analysis of variance procedures. Psychological Bulletin 76(1): 49–57.
Jansen, L.A., and S. Wall. 2009. Paternalism and fairness in clinical research. Bioethics 23(3): 172–182.
Johnson, E.J., and D. Goldstein. 2003. Do defaults save lives? Science 302(5649): 1338–1339.
Korobkin, R. 2009. Libertarian welfarism. California Law Review 97(6): 1651–1685.
Kuczewski, M.G. 1999. Commentary: Narrative views of personal identity and substituted judgment in surrogate decision making. The Journal of Law, Medicine and Ethics 27(1): 32–36.
Lascu, D.-N., W.O. Bearden, and R.L. Rose. 1995. Norm extremity and interpersonal influences on consumer conformity. Journal of Business Research 32(3): 201–212.
Marks, M.A.Z., and H.R. Arkes. 2008. Patient and surrogate disagreement in end-of-life decisions: Can surrogates accurately predict patients’ preferences? Medical Decision Making 28(4): 524–531.
Martin, R., A. Gardikiotis, and M. Hewstone. 2002. Levels of consensus and majority and minority influence. European Journal of Social Psychology 32(5): 645–665.
McKenzie, C.R.M., M.J. Liersch, and S.R. Finkelstein. 2006. Recommendations implicit in policy defaults. Psychological Science 17(5): 414–420.
Ménard, J.-F. 2010. A “nudge” for public health ethics: Libertarian paternalism as a framework for ethical analysis of public health interventions? Public Health Ethics 3(3): 229–238.
Moore, D. 2005. Three in four Americans support euthanasia. The Gallup Organization. Retrieved from http://www.gallup.com/poll/16333/three-four-americans-support-euthanasia.aspx#1.
Nadelhoffer, T., and A. Feltz. 2008. The actor-observer bias and moral intuitions: Adding fuel to Sinnott-Armstrong’s fire. Neuroethics 1(2): 133–144.
Nordholm, L.A. 1975. Effects of group size and stimulus ambiguity on conformity. The Journal of Social Psychology 97(1): 123–130.
Pousset, G., J. Bilsen, J. De Wilde, L. Deliens, and F. Mortier. 2009. Attitudes of Flemish secondary school students towards euthanasia and other end-of-life decisions in minors. Child: Care, Health and Development 35(3): 349–356.
Prendergast, T.J., M.T. Claessens, and J.M. Luce. 1998. A national survey of end-of-life care for critically ill patients. American Journal of Respiratory and Critical Care Medicine 158(4): 1163–1167.
Rachlinski, J.J. 2006. Cognitive errors, individual differences, and paternalism. The University of Chicago Law Review 73: 207–229.
Rencher, A.C., and D.T. Scott. 1990. Assessing the contribution of individual variables following rejection of a multivariate hypothesis. Communication in Statistics: Simulation and Computation 19(2): 535–553.
Rid, A., and D. Wendler. 2010. Can we improve treatment decision-making for incapacitated patients? The Hastings Center Report 40(5): 36–45.
Sadrieh, A., W. Güth, P. Hammerstein, et al. 2002. Group report: Is there evidence for an adaptive toolbox? In Bounded rationality: The adaptive toolbox, ed. G. Gigerenzer and R. Selten, 83–102. Cambridge: MIT Press.
Shalowitz, D.I., E. Garrett-Mayer, and D. Wendler. 2006. The accuracy of surrogate decision makers: A systematic review. Archives of Internal Medicine 166(5): 493–497.
Sharman, S.J., M. Garry, J.A. Jacobson, E.F. Loftus, and P.H. Ditto. 2008. False memories for end-of-life decisions. Health Psychology 27(2): 291–296.
Sulmasy, D.P., P.B. Terry, C.S. Weisman, et al. 1998. The accuracy of substituted judgments in patients with terminal diagnoses. Annals of Internal Medicine 128(8): 621–629.
Sunstein, C.R., and R.H. Thaler. 2003. Libertarian paternalism is not an oxymoron. The University of Chicago Law Review 70: 1159–1202.
Teno, J.M., H.L. Nelson, and J. Lynn. 1994. Advance care planning: Priorities for ethical and empirical research. The Hastings Center Report 24(6): S32–S36.
Thaler, R.H., and C.R. Sunstein. 2008. Nudge: Improving decisions about health, wealth, and happiness. New Haven: Yale University Press.
Todd, P.M., and G. Gigerenzer. 2007. Ecological rationality. Current Directions in Psychological Science 16(3): 167–171.
Torke, A.M., G.A. Sachs, P.R. Helft, et al. 2011. Timing of do-not-resuscitate orders for hospitalized older adults who require a surrogate decision-maker. Journal of American Geriatrics Society 59(7): 1326–1331.
Torke, A.M., M. Siegler, A. Abalos, R.M. Moloney, and G.C. Alexander. 2009. Physicians’ experience with surrogate decision making for hospitalized adults. Journal of General Internal Medicine 24(9): 1023–1028.
Trout, J.D. 2005. Paternalism and cognitive bias. Law and Philosophy 24(4): 393–434.
Uhlmann, R.F., R.A. Pearlman, and K.C. Cain. 1988. Physicians’ and spouses’ predictions of elderly patients’ resuscitation preferences. Journal of Gerontology 43(5): M115–M121.
Weinberg, J.M., S. Nichols, and S. Stich. 2001. Normativity and epistemic intuitions. Philosophical Topics 29(1–2): 429–460.
Williams, N., C. Dunford, A. Knowles, and J. Warner. 2007. Public attitudes to life-sustaining treatments and euthanasia in dementia. International Journal of Geriatric Psychiatry 22(12): 1229–1234.
Wilson, K.G., H.M. Pinocchio, C.J. McPherson, et al. 2007. Desire for euthanasia or physician-assisted suicide in palliative cancer care. Health Psychology 26(3): 314–323.
Acknowledgments
We would like to thank Edward Cokely and two anonymous reviewers for the Journal of Bioethical Inquiry for helpful comments and suggestions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Feltz, A., Samayoa, S. Heuristics and Life-Sustaining Treatments. Bioethical Inquiry 9, 443–455 (2012). https://doi.org/10.1007/s11673-012-9396-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11673-012-9396-5