- 1Faculty of Sports Science, Ningbo University, Ningbo, China
- 2The Affiliated Hospital of Medical School of Ningbo University, Ningbo, China
- 3Department of Sport and Physical Education, Hong Kong Baptist University, Kowloon, Hong Kong SAR, China
Objective: This systematic review aims to make a mixed comparison of interventions for kinesiophobia and individuals with musculoskeletal pain.
Methods: A comprehensive search strategy was conducted in the database of PubMed, MEDLINE, and Web of Science with the inclusion criteria: (1) randomized controlled design; (2) patients with musculoskeletal pain as participants; (3) treatments protocols of kinesiophobia as interventions or comparisons; (4) the score of Tampa Scale Kinesiophobia (TSK) as outcome measures. A network meta-analysis was used to synthesize the data after checking the model consistency. The risk of bias was assessed by the Cochrane Collaboration Risk of Bias Assessment Tool.
Results: Thirty-one studies were included in this review after a comprehensive search strategy with a low risk of bias and good consistency. According to the results of the network meta-analysis, a multi-modal treatment protocol had the highest probability to become the best choice in dealing with kinesiophobia caused by musculoskeletal pain, whereas psychological treatment protocols also showed a potentially positive effect on musculoskeletal pain-induced kinesiophobia.
Conclusion: Multi-modal protocols could be recommended as the preferred option when dealing with kinesiophobia caused by musculoskeletal pain. However, it is still worth mentioning that there are also potentially positive therapeutic effects of psychological interventions. Since the concept of kinesiophobia is based on the fear-avoidance model, the psychological mechanism should be paid enough attention to during treatment.
Registration Number: CRD42021286450.
Introduction
Kinesiophobia, which was firstly proposed by Miller in 1990 based on an aspect of the fear-avoidance model, was a conceptual definition that could describe a fear of pain and an excessive, irrational, and debilitating fear to carry out a physical movement due to a feeling of vulnerability to a painful injury or re-injury (Kori et al., 2011; Vincent et al., 2013; Czuppon et al., 2014; Smith et al., 2014; Monticone et al., 2015; Urquhart et al., 2015; Zdziarski et al., 2015; Ferrándiz et al., 2016; Dvir et al., 2018; Weissenfels et al., 2019; Gholami et al., 2020; Östenberg et al., 2022; Xiang et al., 2022). The developing mechanism of kinesiophobia is multiple and complex, among which the failure and accidents in an individual's movements and the following physical and social activity are the most common. Individuals who are highly fear-avoidant believe that pain is a sign of bodily harm and that any activities causing pain are dangerous and should be avoided (Helmhout et al., 2010; Da Luz et al., 2014). Pain, which might be induced by musculoskeletal disorders, surgeries, and other traumatism, such as burns and scalds, is the most common feature in the progression of kinesiophobia (Galan-Martin et al., 2020; Riecke et al., 2020).
Kinesiophobia induced by musculoskeletal pain is most common and correlates with factors from biological, cognitive, and occupational perspectives (Luque-Suarez et al., 2019). Moreover, kinesiophobia might also occur and develop during the treatment and rehabilitation progression of musculoskeletal disorders, surgeries, and other traumatisms, which call for extra and special intervention (Archer et al., 2017).
The Tampa Scale for Kinesiophobia (TSK) and the Kinesiophobia Causes Scale (KCS) are two common tools being used in the assessment of kinesiophobia. The KCS, which is a questionnaire consisting of 20 close-ended questions with a range of scores from 0 to 100, is usually used to diagnose and determine the causes of motor passivity. Higher scores indicate a greater fear of movement. According to previous studies and evidence-based clinical practice, the TSK is mostly recommended in the assessment of kinesiophobia. For example, a systematic review published in 2004 mentioned that the overall score of TSK showed a significant positive correlation with the severity of the physical disability, and changes in TSK scores could be used as a comparative indicator of treatment effectiveness (Heuts et al., 2004). The original version of TSK is a 17-item questionnaire with the ratings available for each item: (1) disagree; (2) partially disagree; (3) partially agree; (4) strongly agree. The score of each item varies from 1 to 4 or 0 to 3. The score of each item would be summed after the participant finishes the assessment and the overall score ranges from 17 to 68 or from 0 to 51 (Roelofs et al., 2004; Damsgard et al., 2007; Lundberg et al., 2009; Mintken et al., 2010). There are also some shortened versions of TSK with high reliabilities and validities, such as TSK-13 and TSK-11, which have been widely used in the assessment of kinesiophobia caused by pain from other disorders and diseases, such as temporomandibular disorders (TSK-TMD) and chronic low back pain (TSK-CLBP) (Woby et al., 2005; Hapidou et al., 2012; Tkachuk and Harris, 2012; Larsson et al., 2014; Neblett et al., 2016). Moreover, TSK has also been translated into many different languages and has been identified with high test-retest reliability and internal consistency.
The choice of intervention treatment protocol options is an essential part of the treatment for musculoskeletal disorders. Studies of intervention treatment protocols for some musculoskeletal disorders have also found that certain treatments have a positive effect on kinesiophobia caused by pain from these musculoskeletal disorders (Vihstadt et al., 2014; Javdaneh et al., 2020; Tagliaferri et al., 2020). However, since most of the treatment protocols for musculoskeletal disorders are mainly focused on the injured tissues, aiming to restore the physiological functional integrity of damaged tissues, the TSK scores were usually reported as a secondary outcome, and there was a limited number of studies that focus on the treatments for kinesiophobia (Lara-Palomo et al., 2013; Monticone et al., 2017; Sarig Bahat et al., 2018). A systematic review and meta-analysis published in 2020, which only included randomized controlled trials that used the TSK-17 as outcome measures, identified the effect of multi-modal protocols that combined physical and psychological therapies for kinesiophobia caused by musculoskeletal disorders compared with uni-modal therapy of only phycological therapy or psychological therapy, demonstrating that, despite a large heterogeneity within studies, multi-modal protocols might be more effective in reducing kinesiophobia than the unimodal of only physical or psychological therapy (Xu et al., 2020). Therefore, a further review of studies in which more versions of TSK were used as outcome measures should be made to create more comprehensive, high-quality, and low-bias clinical evidence.
At present, there are numerous intervention treatment protocols for musculoskeletal disorders (Flores et al., 2017; Lenoir et al., 2019; Andersen et al., 2020). Therefore, it is not feasible to make an adjusted indirect comparison of interventions or the comparison of a mixed treatment that included every protocol. However, since some protocols just differ in operational details but are based on the same psychophysical principle and could be reclassified together, in this review, each treatment protocol in the studies included would be reclassified according to its operational characteristics and principles, and then put in the network meta-analysis.
According to previous studies, intervention treatment protocols for musculoskeletal disorders could be reclassified into passive modalities (PM), active physical exercise (APE), supervised training (ST), psychological intervention (PI), external-used devices (ED), treatment as usual (TAU), placebo treatment (Placebo), non-intervention (Blank), and multi-modal protocols (MP). In this review, the term PM is defined as therapist-led passive modalities such as acupuncture, manual massage, medication, and therapy using special equipment (laser, ultrasonic wave, magnet, thermal, etc.) (Heymans et al., 2006; Smeets et al., 2009; Ferrándiz et al., 2016; Saracoglu et al., 2020); the term APE refers to interventions in which participants perform physical training in an unsupervised environment or self-training according to a relevant program (resistance training or mobility training), relaxing, or proprioceptive training (Helmhout et al., 2004; Koumantakis et al., 2005; Gustavsson and von Koch, 2006; Pool et al., 2010; Nassif et al., 2011; Monticone et al., 2014; Miyamoto et al., 2016; Hotta et al., 2020); ST refers to physical training by the patient under the supervision of physiotherapists and caregivers (Hott et al., 2020; Meirelles et al., 2020). The term PI refers to treatments conducted by a professional psychologist or psychologist such as cognitive-behavioral therapy (CBT), meditation, and psychological interview (Lopez-Lopez et al., 2015; Monticone et al., 2016, 2018; Zdziarski-Horodyski et al., 2020; Sato et al., 2021), the term ED means the treatment protocol in which the participants would be asked to wear non-invasive therapy devices such as Kinesio tape, orthoses, or sportswear for a long-term (Castro-Sánchez et al., 2012), and the term MP refers to treatment protocols which include two or more protocols mentioned above, for example, physical exercise using VR devices or laser devices. It is important to note that two or more treatments of the same type are not part of a multi-modal protocols program, such as the use of Pilates combined with stretching body exercises in a sports modality (Meijer et al., 2006; Smith et al., 2019; Bahat et al., 2020; Gulsen et al., 2020; Tejera et al., 2020; Javdaneh et al., 2021).
Moreover, the category “Blank” in the reclassification of this review refers to keeping normal life or only receiving patient education with basic health advice (Nassif et al., 2011), whereas the category “TAU” refers to treatment as usual or usual care from nursing staff, and the category “Placebo” refers to sham therapy protocols such as sham manipulation and sham sustained natural apophyseal glides.
The objective of this systematic review is to make a mixed comparison of intervention treatment protocols on kinesiophobia for individuals with musculoskeletal pain by reclassifying treatment protocols from different perspectives according to the change in TSK scores and then to explore the most potential protocols.
Methods
Protocol and Registration
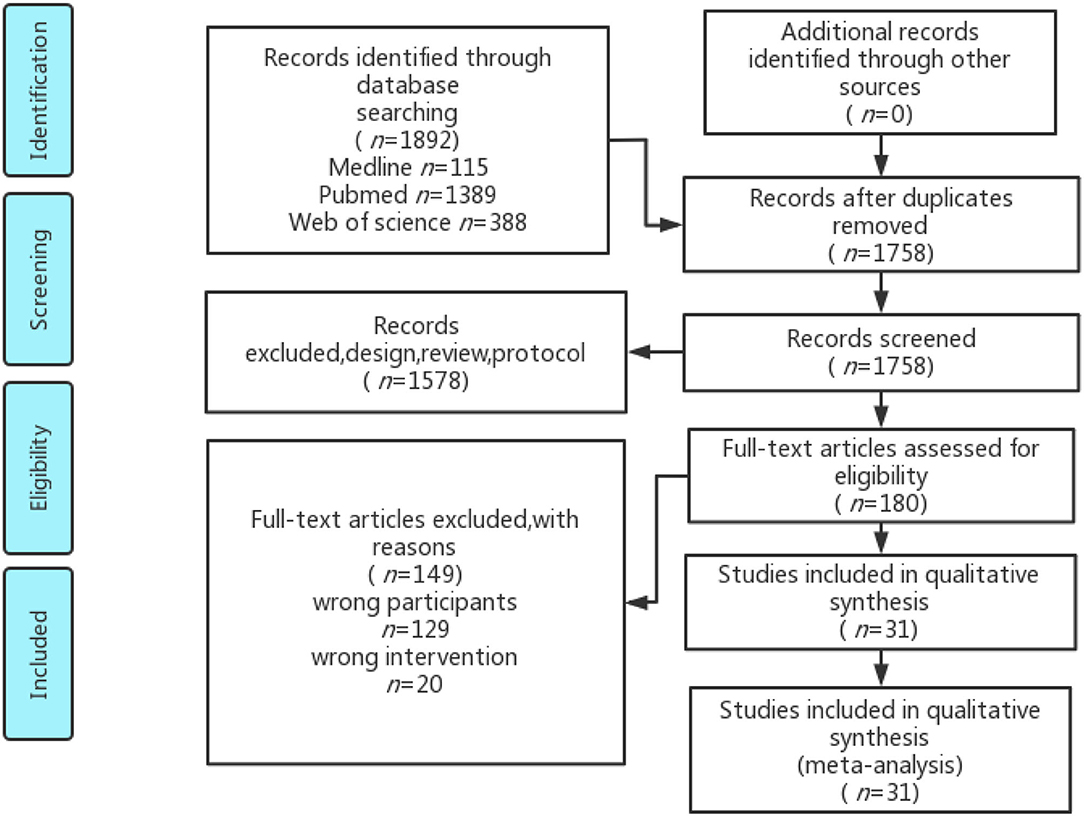
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines (Moher et al., 2009). The eligibility and exclusion criteria and the search strategy were made and agreed upon by two authors (Jialu Huang and Yining Xu) with a priori to minimize bias. The PROSPERO Registration Number of this review is CRD42021286450.
Eligibility Criteria (PICOS)
The eligibility criteria for inclusion were: (1) randomized controlled trials; (2) patients with musculoskeletal pain as participants; (3) intervention treatment protocols; (4) TAU, Placebo, or Blank protocols as comparisons; (5) the score of TSK as outcome measures.
Exclusion Criteria
Studies were excluded if: (1) participants were patients with pain induced by non-musculoskeletal disorders, such as burns, traumatism, or surgeries; (2) intervention protocols contained surgical or invasive treatment such as surgeries and injections; (3) published abstract without full text or lack of data; (4) outcome measures did not correspond with those in the eligibility criteria; (5) not a randomized controlled trial, such as a cross-sectional study, case report, cohort study, and cross-over trial in a single group.
Search Strategy
A comprehensive reproducible search strategy had been performed on the databases of PubMed, MEDLINE, and Web of Science from January 1990 to December 2021. Reference lists were also searched in all screened studies for identifying gray literature, which refers to the study that had not been openly published. If the data were insufficient, the authors were contacted and requested for missing data. The search terms used in each database were as follows: (1) in PubMed and Embase, the search term was “(kinesiophobia) AND [(randomized) OR (randomized)] [Titile/Abstract]”; (2) in Web of Science, the search term was “(AB kinesiophobia) AND (AB randomized OR randomized).”
Risk of Bias Assessment
The risk of bias was assessed by two independent authors (Rongrong Xuan and Julien Baker) according to The Cochrane Collaboration Risk of Bias Assessment Tool (Armijo-Olivo et al., 2012). Every disagreement was discussed, and an independent arbitrator (Yaodong Gu) was invited when there was an agreement that could not be met.
Data Extraction and Synthesis
All searched studies were imported into EndNote 20 (Thomson Reuters, Carlsbad, CA, USA) for further screening. Data were extracted by two independent authors (Jialu Huang and Yining Xu). Any discrepancies would be solved by an independent arbitrator (Yaodong Gu).
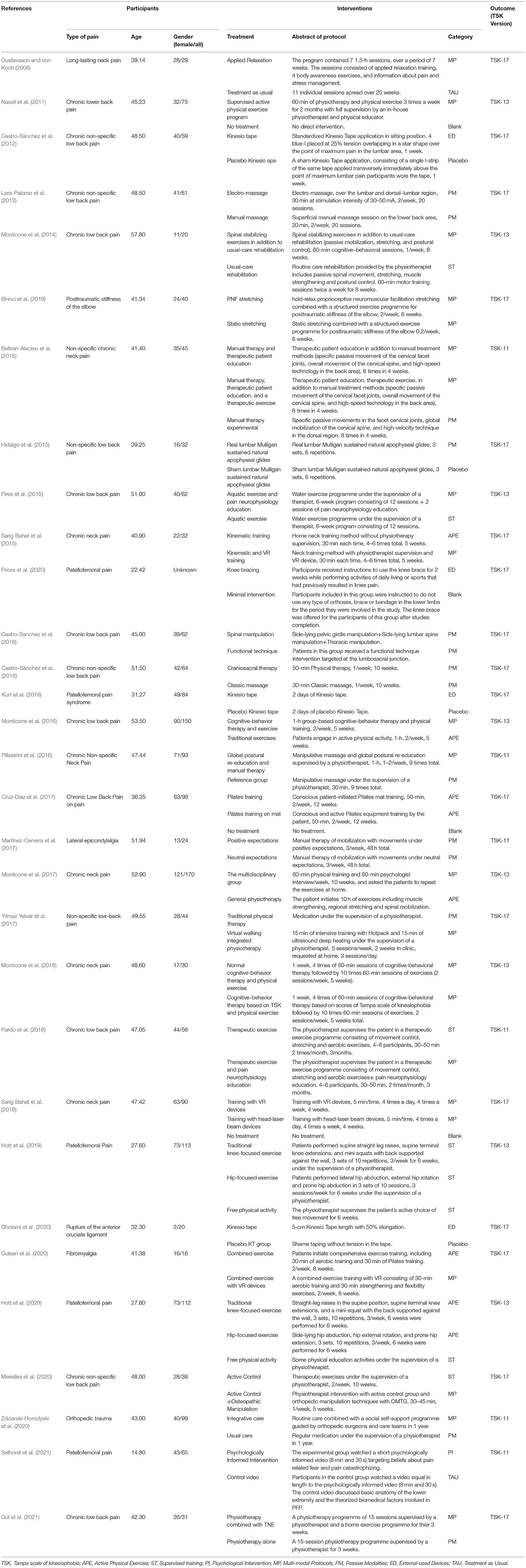
Detailed information of included studies was summarized and information such as participants' characteristics (age, gender, and type of musculoskeletal disorder) and details of intervention protocols with their reclassification were collected and put into an extraction sheet of summary of included studies. The data of each trial, which involved the version of TSK it used, sample size (N), mean value (Mean) with its standard deviation (SD) of each group in baseline, and every recording point would be extracted in an independent sheet for the data pre-processing.
Data Pre-processing
Data pre-processing and analysis were conducted by two independent authors (Jialu Huang and Yining Xu). Microsoft Office Excel (Version 16.0, Microsoft Corporation, Redmond, WA, USA) was used to pre-process the original data by transferring all the outcomes into a uniform unit according to the clinical criteria. The Aggregate Data Drug Information System (ADDIS, Version 1.16.8, Produced by Drugis.org) was used to pool data into the network meta-analysis.
Network Meta-Analysis
Since different versions of TSK have different total scores, the effect size of the network meta-analysis were presented in mean differences (MD) of the percentage of TSK score change. A network geometry was provided to display all kinds of interventions and key information such as the type of intervention represented by each node, direct comparisons between each pair of interventions represented by the edges, and the arms of each comparison which are represented by the number on every edge.
The random-effects standard deviations were calculated under both consistency and inconsistency models and compared with each other to identify if there was inconsistency within interventions. If there were closed loops in the intervention structure, the inconsistency of the evidence must be assessed. Moreover, while the results are easier to interpret, it requires a separate model to be run for each node to be split. The node-splitting analysis is an alternative method to assess inconsistency in network meta-analysis which assessed whether direct and indirect evidence on a specific node (the split node) agrees (Rouse et al., 2017).
The consistency model was used if there was neither closed-loop nor split node in the intervention structure, the random-effects standard deviations in the consistency and inconsistency models were identical, or the identified discrepancy could be determined by examining the calculating a respective Bayesian p-value in the node-splitting analysis was statistically insignificant (p > 0.05). Otherwise, the inconsistency model would be applied (Rouse et al., 2017).
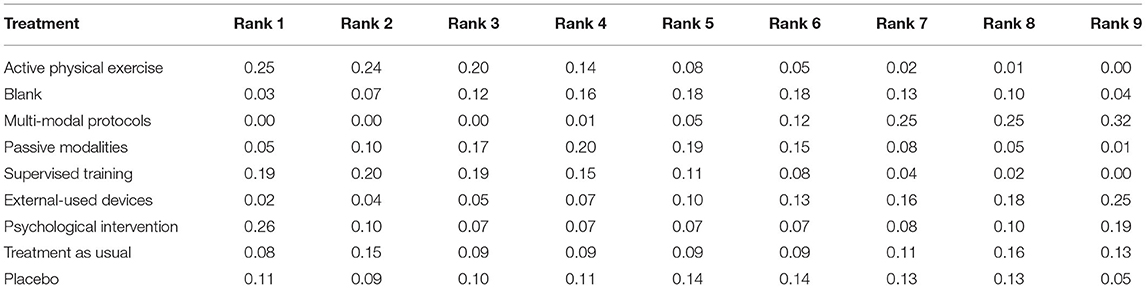
When the consistency model was applied, the results were shown in the rank probability plot. The sum of all rank probabilities is 1, both within a rank over treatments and within a treatment over ranks. Besides, a league table was provided after the model of data analysis had been determined, reporting results that represented the mean difference in the column-defining treatment compared with the row-defining treatment. If the calculation was based on the inconsistency model, only a league table was provided after the model of data analysis had been determined (Catala-Lopez et al., 2014).
Results
Search Strategy and Information Extraction
Thirty-one studies were included in the final analysis (Beltran-Alacreu et al., 2015; Hidalgo et al., 2015; Pires et al., 2015; Sarig Bahat et al., 2015; Castro-Sánchez et al., 2016; Pillastrini et al., 2016; Cruz-Díaz et al., 2017; Martínez-Cervera et al., 2017; Yilmaz Yelvar et al., 2017; Birinci et al., 2019; Gholami et al., 2020). The identification process is shown by a flow diagram in Figure 1 (Moher et al., 2009). The information of all included studies is presented in Table 1. All original data are provided in the Supplementary File.
Risk of Bias
The risk of bias for the 31 included studies was assessed in this review and the results are shown in Figure 2. Adequate results were obtained for the randomization and concealment methods of the participants mentioned in the studies. Eight studies adequately described participants and staff as blind, and a total of 21 studies described assessors as blind. The risk of attrition bias was low (low in all studies), the risk of selection bias was low (low in all studies), and the risk of reporting bias was low (low in all studies).
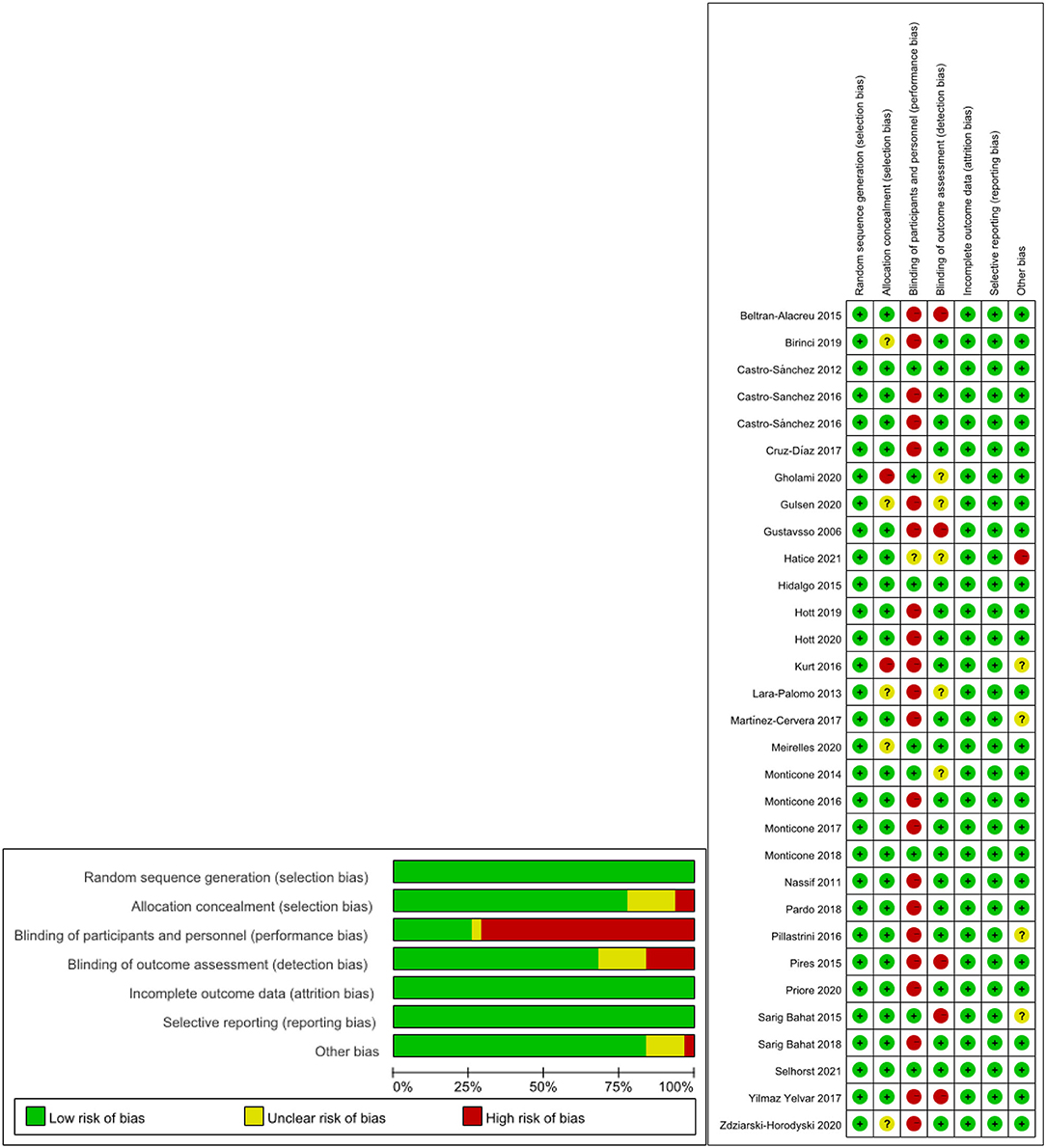
Figure 2. The result of the risk of bias assessment. (A) Risk of bias summary; (B) Risk of bias graph.
Network Meta-Analysis
Network Geometries
The network geometries showed all categories of treatment protocols, providing information such as the type of treatment represented by each node, the direct comparisons between each pair of interventions represented by the lines, and the arms of each trial represented by the number on the edges. The network geometries of the interventions are presented in Figure 3.
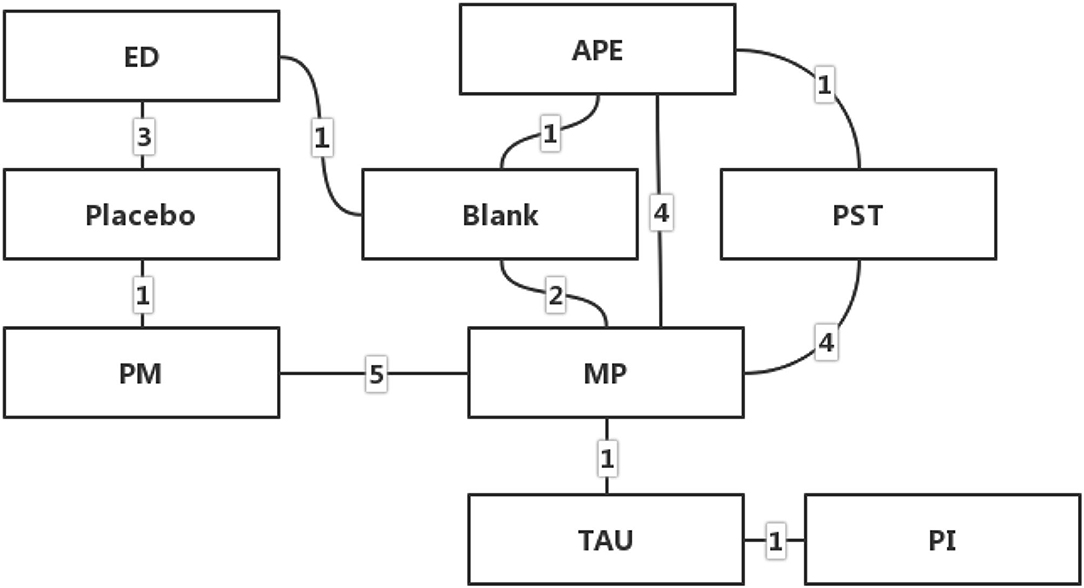
Figure 3. Network geometry of the interventions (APE, Active Physical Exercise; ST, Supervised Training; PI, Psychological Intervention; MP, Multi-modal Protocols; PM, Passive Modalities; ED, External-used Devices; TAU, Treatment as Usual; These figures represent the number of studies that have made direct comparisons between interventions).
Comparisons of Random Effects Standard Deviations
The results of the random effects standard deviation calculations in both the consistency model and inconsistency model of each outcome measure are provided in Table 2. According to the results, the random effects standard deviations of the consistency modal were identical. Therefore, the analysis under the consistency model had a good validity.

Table 2. Random effect standard deviation and 95% confidence interval value of the agreement model and the inconsistency model.
Results of Network Meta-Analysis
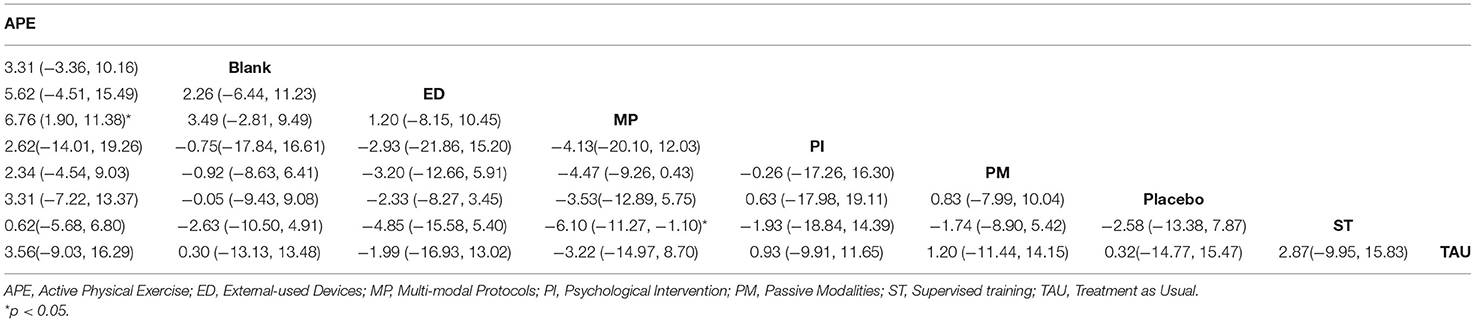
Table 3 shows the league tables of the network geometries, and the ranking of measures and probabilities is provided in Table 4 and Figure 4. Since a lower score of TSK is regarded as better, the treatment protocol in Rank 1 has the highest probability to be the last treatment choice, whereas that in Rank 9 has the lowest probability to be the first treatment choice.
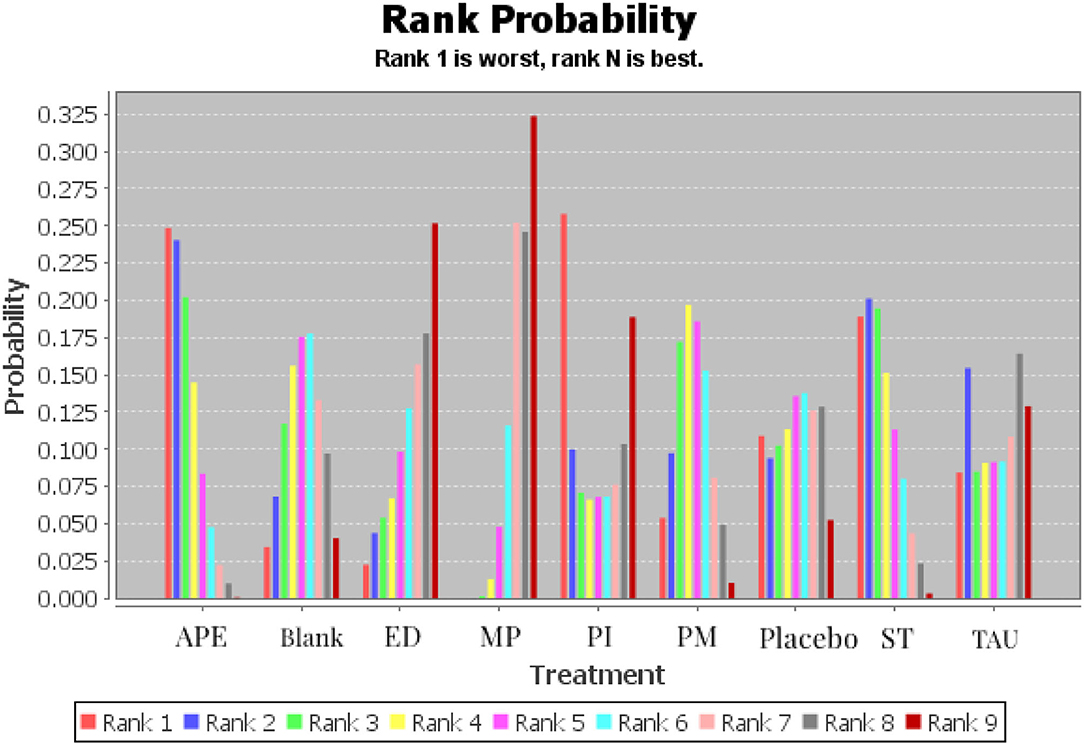
Figure 4. Ranking of measures and probabilities (APE, Active Physical Exercise; ST, Supervised training; PI, Psychological Intervention; MP, Multi-modal Protocols; PM, Passive Modalities; ED, External-used Devices; TAU, Treatment as Usual).
According to the result, MP had the highest potential probability to be the best choice in treating kinesiophobia caused by musculoskeletal pain (0.32 in Rank 9 and 0.25 in Rank 8) with a statistically significant advantage in the comparison with APE (P < 0.05), whereas ED might have the highest potential probability to be the second-best treatment choice with a probability of 0.25 in Rank 9 and 0.18 in Rank 8. The psychological intervention probability is the third-best treatment choice with a probability of 0.19 in Rank 9 and 0.10 in Rank 8. Corresponding with the results of the included studies, TAU and Blank, which were usually set as interventions in the control group, have a high potential probability in Ranks 1 and 2. Nevertheless, APE has the highest potential probability in Ranks 1 and 2.
Discussion
The objective of this systematic review and network meta-analysis is to make a mixed comparison of intervention treatment protocols for kinesiophobia caused by musculoskeletal pain. After comparing 9 different categories of treatment protocols, the primary findings are as follows. First, multi-modal protocols have the highest potential probability to be the best choice in treating kinesiophobia caused by musculoskeletal pain and have a statistically significant advantage in the comparison with active physical exercise and supervised training. Second, wearing an external-used device have the highest potential probability to be the second-best treatment choice. Third, keeping active in physical exercise might not be a wise choice when the patient has been diagnosed with kinesiophobia induced by musculoskeletal pain.
Multi-model treatment protocols seem to have the highest potential probability to be the best treatment choice. This result could be supported by high-level clinical evidence. Apart from the systematic and meta-analysis mentioned in the introduction section of this review (Xu et al., 2020), many randomized controlled trials concluded a similar result to support the clinical practice of multi-disciplinary interventions for kinesiophobia caused by musculoskeletal pain. For example, a pragmatic randomized controlled trial conducted in 2020 claimed that a multi-model treatment protocol combined with nature activity therapy and usual care could be an effective co-adjuvant multicomponent treatment for improving fibromyalgia-related symptoms (Serrat et al., 2020), and another randomized controlled trial conducted in 2013 demonstrated that a long-term multidisciplinary treatment program was superior to the exercise program in reducing disability, fear-avoidance beliefs and pain, as well as enhancing the quality of life of patients with chronic low back pain. The effects were clinically tangible and lasted for at least 1 year after the program ended (Monticone et al., 2013). Moreover, from the non-clinical perspective, a review conducted in 2006, which determined the effectiveness and cost-effectiveness of return-to-work outpatient multidisciplinary treatment programs for sick-listed workers with non-specific upper extremity musculoskeletal complaints, found that multidisciplinary treatment affects individuals positively, but shows no significant difference in cost-effectiveness on the societal level as compared to usual care (Meijer et al., 2006).
The multi-modal treatment protocols included in the review referred to approaches from two or more of the following perspectives, which were physiological, and psychological perspectives. The results of the network meta-analysis showed that the effect of multi-modal treatment protocols was better than that of treatment protocols from only a physiological perspective. This result is correspondent with some previous studies. For example, in a review published in 2014, the therapist performed spinal stabilization exercises based on cognitive behavioral therapy for the patient, and the results showed that spinal stabilization exercises based on cognitive behavioral therapy could bring more advantages to the patient when they were performing non-spinal motor tasks such as walking (Monticone et al., 2014). Another review conducted in 2018 demonstrated that patients with chronic low back pain who were given a pain education session by a psychologist after supervised training by a physiotherapist could feel less pain than those who only had supervised training (Pardo et al., 2018). The results of the network meta-analysis also showed that all multi-modal treatment protocols of the included studies contained treatments from a psychological perspective, indicating that psychological intervention has a potentially positive effect on the kinesiophobia caused by musculoskeletal pain. There is one review included in this study that compares psychological interventions with TAU and finds a significant advantage of psychological intervention over TAU in reducing the severity of kinesiophobia (Selhorst et al., 2021). The results of some previous studies identified the advantage of psychological treatment protocols in treating kinesiophobia induced by musculoskeletal pain and demonstrated that psychological treatment could relieve kinesiophobia caused by physical disorders and improve quality of life (Goudie et al., 2018; Innes et al., 2018; Helminen et al., 2020; Serrat et al., 2020; Xu et al., 2022). For example, a review published in 2016, which has also been included in this systematic review, demonstrated that group-based and task-oriented exercises could reduce disability, kinesiophobia, catastrophizing, and enhance the quality of life of individuals with chronic low back pain (Monticone et al., 2016). Moreover, a review by Wicksell's team, which is a secondary analysis of a randomized controlled trial, resulted in that cognitive behavior therapy could improve the functioning and life satisfaction of people with chronic pain (Wicksell et al., 2010). The potential mechanism of psychological treatments might come from self-efficacy, a review conducted in 2020 shows both pain self-efficacy and negatively charged emotion and expectations toward pain are important factors when dealing with musculoskeletal injured patients (Sinikallio et al., 2014). However, some previous studies concluded different views, a review conducted in 2006 compared the effectiveness of a brief physiotherapy pain management approach using cognitive-behavioral principles with a commonly used method of passive modalities, and identified that the latter approach resulted in higher patient satisfaction overall but the former could be more cost-effective (Moffett et al., 2006). The heterogeneity of the results might be caused by the different expectations of patients when they are selecting treatment protocols. Future studies should compare the effects of different psychological intervention protocols in a particular population to identify the effectiveness of kinesiophobia.
Besides, wearing an externally used device has a high potential probability to be the second-best treatment choice. There are 4 relevant studies included in this review, and 3 studies are randomized controlled trials about the effect of Kinesio tape. For example, a review in 2012 explored the effect of Kinesio tape adhered in the lumbar area, finding that a 1-week treatment of Kinesio tape had a positive effect on relieving pain than the placebo tape (Castro-Sánchez et al., 2012). A review conducted in 2016 evaluated the short-term effects of Kinesio tape on joint position sense, isokinetic measurements, kinesiophobia, symptoms, and functional limitations in patients with patellofemoral pain syndrome, demonstrating that, although short-term Kinesio tape application could not increase hamstring muscle strength, it still could improve joint position sense, pain, kinesiophobia, symptoms, and daily limitations (Kurt et al., 2016). The positive effect of the Kinesio tape application has been identified by several previous studies (Coombes et al., 2016; Karran et al., 2017; Louw et al., 2017; Takacs et al., 2017); however, most of these studies only identified the short-term effect of Kinesio tape. Further studies should identify the long-term effect of Kinesio tape and that of other kinds of externally used therapy devices.
What should also be noticed among the results of the network meta-analysis is that, for the treatment of kinesiophobia caused by musculoskeletal pain, active physical exercise might not be recommended with the lowest potential, which seems even lower than placebo, within the 9 treatment protocol categories. The reason might come from two possible aspects. First, active physical exercise might lead to secondary injury and further pain. Second, this result might be caused by the heterogeneity of intervention protocols in these included studies. Therefore, the interpretation of this result should be cautious, and future studies should explore the effect of active physical exercise on kinesiophobia without covariate interference.
Within all 9 categories of treatment protocols, TAU and Blank, which were usually set as interventions in the control group, have a low potential probability to have a positive effect on kinesiophobia caused by musculoskeletal pain. It is because treatment as usual and no-treatment, themselves are not clinical treatment protocols, only being set as interventions in control groups in the included studies. Besides, this result could also indicate that kinesiophobia might not be a self-limiting disease whose symptoms would not resolve themselves over time. It means that if patients with kinesiophobia do not carry out a particular treatment, only usual care would not be effective on their symptoms.
The primary limitation of this systematic review is that there is a limited number of studies that focus on the treatments for kinesiophobia, leading to a lack of arms in some direct intervention comparisons. For example, there is no direct comparison between psychological intervention and externally used devices in the network geometry. Last but not least, the score of TSK is usually reported as a secondary outcome, resulting in publication bias to some extent (Bennell et al., 2020; Öztürk et al., 2021; Serrat et al., 2021).
Conclusion
Multi-modal protocols could be recommended as the preferred option when dealing with kinesiophobia caused by musculoskeletal pain. However, it is still worth mentioning that there are also potentially positive therapeutic effects of psychological interventions. Since the concept of kinesiophobia is based on the fear-avoidance model, the psychological mechanism should be paid enough attention to during treatment.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Materials, further inquiries can be directed to the corresponding authors.
Author Contributions
JH conceived the study design, collected and analyzed data, and drafted the manuscript. YX and RX participated in the design of the study, collected, and analyzed data. YG, RX, and JB conceived the study design, assisted in revising the manuscript, and reviewed the first and final versions of the manuscript. All authors contributed to the article and agreed to the submitted version of the manuscript.
Funding
This study was supported by Zhejiang Province Medical and Health Science and Technology Plan Project (No. 2018KY710), Ningbo Public Welfare Science and Technology Plan Project (No. 2019C50095), Health Youth Technical Talent Cultivation Special Fund Project (2020SWSQNGG-01), Ningbo Medical Science and Technology Plan (2020Y14), and Young Cultivation Fund Project of the Affiliated of School of Medicine of Ningbo University (FYQM-KY-202003).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2022.886015/full#supplementary-material
References
Andersen, T. E., Ellegaard, H., Schiottz-Christensen, B., Mejldal, A., and Manniche, C. (2020). Somatic experiencing for patients with low back pain and comorbid posttraumatic stress symptoms - a randomised controlled trial. Eur. J. Psychotraumatol. 11, 1797306. doi: 10.1080/20008198.2020.1797306
Archer, K. R., Devin, C. J., Vanston, S. W., Koyama, T., Phillips, S. E., Mathis, S. L., et al. (2017). Cognitive-behavioral-based physical therapy for patients with chronic pain undergoing lumbar spine surgery: a randomized controlled trial. J. Pain 18, 477. doi: 10.1016/j.jpain.2017.02.425
Armijo-Olivo, S., Stiles, C. R., Hagen, N. A., Biondo, P. D., and Cummings, G. G. (2012). Assessment of study quality for systematic reviews: a comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: methodological research. J. Eval. Clin. Pract. 18, 12–18. doi: 10.1111/j.1365-2753.2010.01516.x
Bahat, H. S., Hadar, D., and Treleaven, J. (2020). Predictors for positive response to home kinematic training in chronic neck pain. J. Manipulative Physiol. Ther. 43, 779–790. doi: 10.1016/j.jmpt.2019.12.008
Beltran-Alacreu, H., López-de-Uralde-Villanueva, I., Fernández-Carnero, J., and La Touche, R. (2015). Manual therapy, therapeutic patient education, and therapeutic exercise, an effective multimodal treatment of nonspecific chronic neck pain: a randomized controlled trial. Am. J. Phys. Med. Rehabil. 94(10 Suppl. 1), 887–897. doi: 10.1097/phm.0000000000000293
Bennell, K., Nelligan, R. K., Schwartz, S., Kasza, J., Kimp, A., Crofts, S. J. C., et al. (2020). Behavior change text messages for home exercise adherence in knee osteoarthritis: randomized trial. J. Med. Internet Res. 22, 868–878. doi: 10.2196/21749
Birinci, T., Razak Ozdincler, A., Altun, S., and Kural, C. (2019). A structured exercise programme combined with proprioceptive neuromuscular facilitation stretching or static stretching in posttraumatic stiffness of the elbow: a randomized controlled trial. Clin. Rehabil. 33, 241–252. doi: 10.1177/0269215518802886
Castro-Sanchez, A. M., Lara-Palomo, I. C., Mataran-Penarrocha, G. A., Fernandez-De-Las-Penas, C., Saavedra-Hernandez, M., Cleland, J., et al. (2016). Short-term effectiveness of spinal manipulative therapy versus functional technique in patients with chronic nonspecific low back pain: a pragmatic randomized controlled trial. Spine J. 16, 302–312. doi: 10.1016/j.spinee.2015.08.057
Castro-Sánchez, A. M., Lara-Palomo, I. C., Matarán-Peñarrocha, G. A., Fernández-Sánchez, M., Sánchez-Labraca, N., and Arroyo-Morales, M. (2012). Kinesio taping reduces disability and pain slightly in chronic non-specific low back pain: a randomised trial. J. Physiother. 58, 89–95. doi: 10.1016/s1836-9553(12)70088-7
Castro-Sánchez, A. M., Lara-Palomo, I. C., Matarán-Peñarrocha, G. A., Saavedra-Hernández, M., Pérez-Mármol, J. M., and Aguilar-Ferrándiz, M. E. (2016). Benefits of craniosacral therapy in patients with chronic low back pain: a randomized controlled trial. J. Altern. Complement. Med. 22, 650–657. doi: 10.1089/acm.2016.0068
Catala-Lopez, F., Tobias, A., Cameron, C., Moher, D., and Hutton, B. (2014). Network meta-analysis for comparing treatment effects of multiple interventions: an introduction. Rheumatol. Int. 34, 1489–1496. doi: 10.1007/s00296-014-2994-2
Coombes, B. K., Wiebusch, M., Heales, L., Stephenson, A., and Vicenzino, B. (2016). Isometric exercise above but not below an individual's pain threshold influences pain perception in people with lateral epicondylalgia. Clin. J. Pain 32, 1069–1075. doi: 10.1097/AJP.0000000000000365
Cruz-Díaz, D., Bergamin, M., Gobbo, S., Martínez-Amat, A., and Hita-Contreras, F. (2017). Comparative effects of 12 weeks of equipment based and mat Pilates in patients with Chronic Low Back Pain on pain, function and transversus abdominis activation. A randomized controlled trial. Complement. Ther. Med. 33, 72–77. doi: 10.1016/j.ctim.2017.06.004
Czuppon, S., Racette, B. A., Klein, S. E., and Harris-Hayes, M. (2014). Variables associated with return to sport following anterior cruciate ligament reconstruction: a systematic review. Br. J. Sports Med. 48, 356–364. doi: 10.1136/bjsports-2012-091786
Da Luz, M. A., Costa, L. O. P., Fuhro, F. F., Manzoni, A. C. T., Oliveira, N. T. B., and Cabral, C. M. N. (2014). Effectiveness of mat pilates or equipment-based pilates exercises in patients with chronic nonspecific low back pain: a randomized controlled trial. Phys. Ther. 94, 623–631. doi: 10.2522/ptj.20130277
Damsgard, E., Fors, T., Anke, A., and Roe, C. (2007). The Tampa Scale of Kinesiophobia: a Rasch analysis of its properties in subjects with low back and more widespread pain. J. Rehabil. Med. 39, 672–678. doi: 10.2340/16501977-0125
Dvir, Y., Levant, A., Efimov, D., Polyakov, A., and Perruquetti, W. (2018). Acceleration of finite-time stable homogeneous systems. Int. J. Robust. Nonlin Cont. 28, 1757–1777. doi: 10.1002/rnc.3984
Ferrándiz, M. E. A., Nijs, J., Gidron, Y., Roussel, N., Vanderstraeten, R., Van Dyck, D., et al. (2016). Auto-targeted neurostimulation is not superior to placebo in chronic low back pain: a fourfold blind randomized clinical trial. Pain Phys. 19, E707–E719. doi: 10.36076/ppj/2019.19.E707
Flores, C., Balius, R., Álvarez, G., Buil, M. A., Varela, L., Cano, C., et al. (2017). Efficacy and tolerability of peritendinous hyaluronic acid in patients with supraspinatus tendinopathy: a multicenter, randomized, controlled trial. Sports Med Open 3, 22. doi: 10.1186/s40798-017-0089-9
Galan-Martin, M. A., Montero-Cuadrado, F., Lluch-Girbes, E., Coca-López, M. C., Mayo-Iscar, A., and Cuesta-Vargas, A. (2020). Pain neuroscience education and physical therapeutic exercise for patients with chronic spinal pain in spanish physiotherapy primary care: a pragmatic randomized controlled trial. J. Clin. Med. 9, 1201. doi: 10.3390/jcm9041201
Gholami, M., Kamali, F., Mirzeai, M., Motealleh, A., and Shamsi, M. (2020). Effects of kinesio tape on kinesiophobia, balance and functional performance of athletes with post anterior cruciate ligament reconstruction: a pilot clinical trial. BMC Sports Sci. Med. Rehabil. 12, 57. doi: 10.1186/s13102-020-00203-x
Goudie, S., Dixon, D., McMillan, G., Ring, D., and McQueen, M. (2018). Is use of a psychological workbook associated with improved disabilities of the arm, shoulder and hand scores in patients with distal radius fracture? Clin. Orthop. Relat. Res. 476, 832–845. doi: 10.1007/s11999.0000000000000095
Gül, H., Erel, S., and Toraman, N. F. (2021). Physiotherapy combined with therapeutic neuroscience education versus physiotherapy alone for patients with chronic low back pain: a pilot, randomized-controlled trial. Turk. J. Phys. Med. Rehabil. 67, 283. doi: 10.5606/tftrd.2021.5556
Gulsen, C. P. T. M., Soke, F. P. T. P., Eldemir, K. P. T. M., Apaydin, Y. P. T. M., Ozkul, C. P. T. P., Guclu-Gunduz, A. P. T. P., et al. (2020). Effect of fully immersive virtual reality treatment combined with exercise in fibromyalgia patients: a randomized controlled trial. Assistive Technol. 34, 1–8. doi: 10.1080/10400435.2020.1772900
Gustavsson, C., and von Koch, L. (2006). Applied relaxation in the treatment of long-lasting neck pain: a randomized controlled pilot study. J. Rehabil. Med. 38, 100–107. doi: 10.1080/16501970510044025
Hapidou, E. G., O'Brien, M. A., Pierrynowski, M. R., de Las Heras, E., Patel, M., and Patla, T. (2012). Fear and avoidance of movement in people with chronic pain: psychometric properties of the 11-item tampa scale for kinesiophobia (TSK-11). Physiother. Can. 64, 235–241. doi: 10.3138/ptc.2011-10
Helmhout, P. H., Harts, C. C., Staal, J. B., Candel, M. J. J. M., and de Bie, R. A. (2004). Comparison of a high-intensity and a low-intensity lumbar extensor training program as minimal intervention treatment in low back pain: a randomized trial. Euro. Spine J. 13, 537–547. doi: 10.1007/s00586-004-0671-y
Helmhout, P. H., Staal, J. B., Heymans, M. W., Harts, C. C., Hendriks, E. J. M., and de Bie, R. A. (2010). Prognostic factors for perceived recovery or functional improvement in non-specific low back pain: secondary analyses of three randomized clinical trials. Euro. Spine J. 19, 650–659. doi: 10.1007/s00586-009-1254-8
Helminen, E.-E., Arokoski, J. P., Selander, T. A., and Sinikallio, S. H. (2020). Multiple psychological factors predict pain and disability among community-dwelling knee osteoarthritis patients: a five-year prospective study. Clin. Rehabil. 34, 404–415. doi: 10.1177/0269215519900533
Heuts, P. H., Vlaeyen, J. W., Roelofs, J., de Bie, R. A., Aretz, K., van Weel, C., et al. (2004). Pain-related fear and daily functioning in patients with osteoarthritis. Pain 110, 228–235. doi: 10.1016/j.pain.2004.03.035
Heymans, M. W., de Vet, H. C. W., Bongers, P. M., Knol, D. L., Koes, B. W., and van Mechelen, W. (2006). The effectiveness of high-intensity versus low-intensity back schools in an occupational setting: a pragmatic randomized controlled trial. Spine. 31, 1075–1082. doi: 10.1097/01.brs.0000216443.46783.4d
Hidalgo, B., Pitance, L., Hall, T., Detrembleur, C., and Nielens, H. (2015). Short-term effects of Mulligan mobilization with movement on pain, disability, and kinematic spinal movements in patients with nonspecific low back pain: a randomized placebo-controlled trial. J. Manipulative Physiol. Ther. 38, 365–374. doi: 10.1016/j.jmpt.2015.06.013
Hott, A., Brox, J. I., Pripp, A. H., Juel, N. G., and Liavaag, S. (2020). Patellofemoral pain: One year results of a randomized trial comparing hip exercise, knee exercise, or free activity. Scand. J. Med. Sci. Sports 30, 741–753. doi: 10.1111/sms.13613
Hott, A., Brox, J. I., Pripp, A. H., Juel, N. G., Paulsen, G., and Liavaag, S. (2019). Effectiveness of isolated hip exercise, knee exercise, or free physical activity for patellofemoral pain: a randomized controlled trial. Am. J. Sports Med. 47, 1312–1322. doi: 10.1177/0363546519830644
Hotta, G. H., Gomes de Assis Couto, A., Cools, A. M., McQuade, K. J., and Siriani de Oliveira, A. (2020). Effects of adding scapular stabilization exercises to a periscapular strengthening exercise program in patients with subacromial pain syndrome: a randomized controlled trial. Musculoskelet Sci. Pract. 49, 102171. doi: 10.1016/j.msksp.2020.102171
Innes, K. E., Selfe, T. K., Kandati, S., Wen, S. J., and Huysmans, Z. (2018). Effects of mantra meditation versus music listening on knee pain, function, and related outcomes in older adults with knee osteoarthritis: an exploratory randomized clinical trial (RCT). Evid. Based Complement. Alternat. Med. 2018, 19. doi: 10.1155/2018/7683897
Javdaneh, N., Letafatkar, A., Shojaedin, S., and Hadadnezhad, M. (2020). Scapular exercise combined with cognitive functional therapy is more effective at reducing chronic neck pain and kinesiophobia than scapular exercise alone: a randomized controlled trial. Clin. Rehabil. 34, 1485–1496. doi: 10.1177/0269215520941910
Javdaneh, N., Saeterbakken, A. H., Shams, A., and Barati, A. H. (2021). Pain neuroscience education combined with therapeutic exercises provides added benefit in the treatment of chronic neck pain. Int. J. Environ. Res. Public Health 18, 1485–1496. doi: 10.3390/ijerph18168848
Karran, E. L., Medalian, Y., Hillier, S. L., and Moseley, G. L. (2017). The impact of choosing words carefully: an online investigation into imaging reporting strategies and best practice care for low back pain. PeerJ 5, e4151. doi: 10.7717/peerj.4151
Kori, S. H., Miller, R. P., and Todd, D. D. J. P. M. (2011). Kinisophobia: A new view of chronic pain behavior. J. Hum. Kinet. 28, 25–31. doi: 10.2478/v10078-011-0019-8
Koumantakis, G. A., Watson, P. J., and Oldham, J. A. (2005). Trunk muscle stabilization training plus general exercise versus general exercise only: randomized controlled trial of patients with recurrent low back pain. Phys. Ther. 85, 209–225. doi: 10.1093/ptj/85.3.209
Kurt, E. E., Büyükturan, Ö., Erdem, H. R., Tuncay, F., and Sezgin, H. (2016). Short-term effects of kinesio tape on joint position sense, isokinetic measurements, and clinical parameters in patellofemoral pain syndrome. J. Phys. Ther. Sci. 28, 2034–2040. doi: 10.1589/jpts.28.2034
Lara-Palomo, I. C., Aguilar-Ferrándiz, M. E., Matarán-Peñarrocha, G. A., Saavedra-Hernández, M., Granero-Molina, J., Fernández-Sola, C., et al. (2013). Short-term effects of interferential current electro-massage in adults with chronic non-specific low back pain: a randomized controlled trial. Clin. Rehabil. 27, 439–449. doi: 10.1177/0269215512460780
Larsson, C., Hansson, E. E., Sundquist, K., and Jakobsson, U. (2014). Psychometric properties of the Tampa Scale of Kinesiophobia (TSK-11) among older people with chronic pain. Physiother. Theory Pract. 30, 421–428. doi: 10.3109/09593985.2013.877546
Lenoir, D., Coppieters, I., Willaert, W., Kregel, J., Danneels, L., Cagnie, B., et al. (2019). Do sociodemographic features, pain sensitivity or pain catastrophizing relate to clinic-based adherence to physiotherapy in people suffering from chronic spinal pain? Secondary analysis of a randomized clinical trial. Musculoskelet Sci. Pract. 44, 102066. doi: 10.1016/j.msksp.2019.102066
Lopez-Lopez, A., Alonso Perez, J. L., González Gutierez, J. L., La Touche, R., Lerma Lara, S., Izquierdo, H., et al. (2015). Mobilization versus manipulations versus sustain apophyseal natural glide techniques and interaction with psychological factors for patients with chronic neck pain: randomized controlled trial. Euro. J. Phys. Rehabil. Med. 51, 121–132.
Louw, A., Puentedura, E. J., Reese, D., Parker, P., Miller, T., and Mintken, P. E. (2017). Immediate effects of mirror therapy in patients with shoulder pain and decreased range of motion. Arch. Phys. Med. Rehabil. 98, 1941–1947. doi: 10.1016/j.apmr.2017.03.031
Lundberg, M., Styf, J., and Jansson, B. (2009). On what patients does the Tampa Scale for kinesiophobia fit? Physiother. Theory Pract. 25, 495–506. doi: 10.3109/09593980802662160
Luque-Suarez, A., Martinez-Calderon, J., and Falla, D. (2019). Role of kinesiophobia on pain, disability and quality of life in people suffering from chronic musculoskeletal pain: a systematic review. Br. J. Sports Med. 53, 554–559. doi: 10.1136/bjsports-2017-098673
Martínez-Cervera, F. V., Olteanu, T. E., Gil-Martínez, A., Díaz-Pulido, B., and Ferrer-Peña, R. (2017). Influence of expectations plus mobilization with movement in patient with lateral epicondylalgia: a pilot randomized controlled trial. J. Exerc. Rehabil. 13, 101–109. doi: 10.12965/jer.1732848.424
Meijer, E. M., Sluiter, J. K., Heyma, A., Sadiraj, K., and Frings-Dresen, M. H. W. (2006). Cost-effectiveness of multidisciplinary treatment in sick-listed patients with upper extremity musculoskeletal disorders: a randomized, controlled trial with one-year follow-up. Int. Arch. Occup. Environ. Health 79, 654–664. doi: 10.1007/s00420-006-0098-3
Meirelles, F. D., Cunha, J., and da Silva, E. B. (2020). Osteopathic manipulation treatment versus therapeutic exercises in patients with chronic nonspecific low back pain: a randomized, controlled and double-blind study. J. Back Musculoskelet. Rehabil. 33, 367–377. doi: 10.3233/BMR-181355
Mintken, P. E., Cleland, J. A., Whitman, J. M., and George, S. Z. (2010). Psychometric properties of the Fear-Avoidance Beliefs Questionnaire and Tampa Scale of Kinesiophobia in patients with shoulder pain. Arch. Phys. Med. Rehabil. 91, 1128–1136. doi: 10.1016/j.apmr.2010.04.009
Miyamoto, G. C., Moura, K. F., dos Santos Franco, Y. R., de Oliveira, N. T. B., Amaral, D. D. V., et al. (2016). Effectiveness and cost-effectiveness of different weekly frequencies of pilates for chronic low back pain: randomized controlled trial. Phys. Ther. 96, 382–389. doi: 10.2522/ptj.20150404
Moffett, J. K., Jackson, D. A., Gardiner, E. D., Torgerson, D. J., Coulton, S., Eaton, S., et al. (2006). Randomized trial of two physiotherapy interventions for primary care neck and back pain patients: 'McKenzie' vs brief physiotherapy pain management. Rheumatology 45, 1514–1521. doi: 10.1093/rheumatology/kel339
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., and Group, P. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339, b2535. doi: 10.1136/bmj.b2535
Monticone, M., Ambrosini, E., Rocca, B., Cazzaniga, D., Liquori, V., and Foti, C. (2016). Group-based task-oriented exercises aimed at managing kinesiophobia improved disability in chronic low back pain. Eur. J. Pain 20, 541–551. doi: 10.1002/ejp.756
Monticone, M., Ambrosini, E., Rocca, B., Cazzaniga, D., Liquori, V., Pedrocchi, A., et al. (2017). Group-based multimodal exercises integrated with cognitive-behavioural therapy improve disability, pain and quality of life of subjects with chronic neck pain: a randomized controlled trial with one-year follow-up. Clin. Rehabil. 31, 742–752. doi: 10.1177/0269215516651979
Monticone, M., Ambrosini, E., Rocca, B., Magni, S., Brivio, F., and Ferrante, S. (2014). A multidisciplinary rehabilitation programme improves disability, kinesiophobia and walking ability in subjects with chronic low back pain: results of a randomised controlled pilot study. Eur. Spine J. 23, 2105–2113. doi: 10.1007/s00586-014-3478-5
Monticone, M., Ambrosini, E., Vernon, H., Rocca, B., Finco, G., Foti, C., et al. (2018). Efficacy of two brief cognitive-behavioral rehabilitation programs for chronic neck pain: results of a randomized controlled pilot study. Eur. J. Phys. Rehabil. Med. 54, 890–899. doi: 10.23736/S1973-9087.18.05206-1
Monticone, M., Cedraschi, C., Ambrosini, E., Rocca, B., Fiorentini, R., Restelli, M., et al. (2015). Cognitive-behavioural treatment for subacute and chronic neck pain. Cochrane Database Syst. Rev. 2015, CD010664. doi: 10.1002/14651858.CD010664.pub2
Monticone, M., Ferrante, S., Rocca, B., Baiardi, P., Dal Farra, F., and Foti, C. (2013). Effect of a long-lasting multidisciplinary program on disability and fear-avoidance behaviors in patients with chronic low back pain: results of a randomized controlled trial. Clin. J. Pain 11, 929–938. doi: 10.1097/AJP.0b013e31827fef7e
Nassif, H., Brosset, N., Guillaume, M., Delore-Milles, E., Tafflet, M., Buchholz, F., et al. (2011). Evaluation of a randomized controlled trial in the management of chronic lower back pain in a French automotive industry: an observational study. Arch. Phys. Med. Rehabil. 92, 1927–1936.e1924. doi: 10.1016/j.apmr.2011.06.029
Neblett, R., Hartzell, M. M., Mayer, T. G., Bradford, E. M., and Gatchel, R. J. (2016). Establishing clinically meaningful severity levels for the Tampa Scale for Kinesiophobia (TSK-13). Eur. J. Pain 20, 701–710. doi: 10.1002/ejp.795
Östenberg, A. H., Pojskic, H., Gilic, B., Sekulic, D., and Alricsson, M. (2022). Physical fitness, dietary habits and substance misuse: a cross-sectional analysis of the associations in 7,600 swedish adolescents. Phys. Activity Health 6, 26–37. doi: 10.5334/paah.164
Öztürk, Ö., Bombac,i, H., Keçeci, T., and Algun, Z.C. (2021). Effects of additional action observation to an exercise program in patients with chronic pain due to knee osteoarthritis: a randomized-controlled trial. Musculoskelet Sci. Pract. 52, 102334. doi: 10.1016/j.msksp.2021.102334
Pardo, G. B., Girbes, E. L., Roussel, N. A., Izquierdo, T. G., Penick, V. J., and Martin, D. P. (2018). Pain neurophysiology education and therapeutic exercise for patients with chronic low back pain: a single-blind randomized controlled trial. Arch. Phys. Med. Rehabil. 99, 338–347. doi: 10.1016/j.apmr.2017.10.016
Pillastrini, P., Resende, F., Banchelli, F., Burioli, A., Di Ciaccio, E., Guccione, A. A., et al. (2016). Effectiveness of global postural re-education in patients with chronic nonspecific neck pain: randomized controlled trial. Phys. Ther. 96, 1408–1416. doi: 10.2522/ptj.20150501
Pires, D., Cruz, E. B., and Caeiro, C. (2015). Aquatic exercise and pain neurophysiology education versus aquatic exercise alone for patients with chronic low back pain: a randomized controlled trial. Clin. Rehabil. 29, 538–547. doi: 10.1177/0269215514549033
Pool, J. J. M., Ostelo, R. W. J. G., Knol, D. L., Vlaeyen, J. W. S., Bouter, L. M., and de Vet, H. C. W. (2010). Is a behavioral graded activity program more effective than manual therapy in patients with subacute neck pain? Results of a randomized clinical trial. Spine 35, 1017–1024. doi: 10.1097/BRS.0b013e3181c212ee
Priore, L. B., Lack, S., Garcia, C., Azevedo, F. M., and de Oliveira Silva, D. (2020). Two weeks of wearing a knee brace compared with minimal intervention on kinesiophobia at 2 and 6 weeks in people with patellofemoral pain: a randomized controlled trial. Arch. Phys. Med. Rehabil. 101, 613–623. doi: 10.1016/j.apmr.2019.10.190
Riecke, J., Rief, W., Vlaeyen, J. W. S., and Glombiewski, J. A. (2020). Generalizability of harm and pain expectations after exposure in chronic low back pain patients. Euro. J. Pain 24, 1495–1504. doi: 10.1002/ejp.1604
Roelofs, J., Goubert, L., Peters, M. L., Vlaeyen, J. W., and Crombez, G. (2004). The Tampa Scale for Kinesiophobia: further examination of psychometric properties in patients with chronic low back pain and fibromyalgia. Eur. J. Pain 8, 495–502. doi: 10.1016/j.ejpain.2003.11.016
Rouse, B., Chaimani, A., and Li, T. (2017). Network meta-analysis: an introduction for clinicians. Intern. Emerg. Med. 12, 103–111. doi: 10.1007/s11739-016-1583-7
Saracoglu, I., Arik, M. I., Afsar, E., and Gokpinar, H. H. (2020). The effectiveness of pain neuroscience education combined with manual therapy and home exercise for chronic low back pain: a single-blind randomized controlled trial. Physiother. Theory Pract. 38, 1–11. doi: 10.1080/09593985.2020.1809046
Sarig Bahat, H., Croft, K., Carter, C., Hoddinott, A., Sprecher, E., and Treleaven, J. (2018). Remote kinematic training for patients with chronic neck pain: a randomised controlled trial. Eur. Spine J. 27, 1309–1323. doi: 10.1007/s00586-017-5323-0
Sarig Bahat, H., Takasaki, H., Chen, X., Bet-Or, Y., and Treleaven, J. (2015). Cervical kinematic training with and without interactive VR training for chronic neck pain - a randomized clinical trial. Man. Ther. 20, 68–78. doi: 10.1016/j.math.2014.06.008
Sato, T., Shimizu, K., Shiko, Y., Kawasaki, Y., Orita, S., Inage, K., et al. (2021). Effects of nintendo ring fit adventure exergame on pain and psychological factors in patients with chronic low back pain. Games Health J. 10, 158–164. doi: 10.1089/g4h.2020.0180
Selhorst, M., Fernandez-Fernandez, A., Schmitt, L., and Hoehn, J. (2021). Effect of a psychologically informed intervention to treat adolescents with patellofemoral pain: a randomized controlled trial. Arch. Phys. Med. Rehabil. 102, 1267–1273. doi: 10.1016/j.apmr.2021.03.016
Serrat, M., Almirall, M., Must,é, M., Sanabria-Mazo, J. P., Feliu-Soler, A., Méndez-Ulrich, J. L., et al. (2020). Effectiveness of a multicomponent treatment for fibromyalgia based on pain neuroscience education, exercise therapy, psychological support, and nature exposure (NAT-FM): a pragmatic randomized controlled trial. J. Clin. Med. 9, 3348. doi: 10.3390/jcm9103348
Serrat, M., Coll-Omaña, M., Albajes, K., Sol,é, S., Almirall, M., Luciano, J. V., et al. (2021). Efficacy of the FIBROWALK multicomponent program moved to a virtual setting for patients with fibromyalgia during the COVID-19 pandemic: a proof-of-concept RCT performed alongside the state of alarm in Spain. Int. J. Environ. Res. Public Health 18. doi: 10.3390/ijerph181910300
Sinikallio, S. H., Helminen, E. E., Valjakka, A. L., Vaisanen-Rouvali, R. H., and Arokoski, J. P. (2014). Multiple psychological factors are associated with poorer functioning in a sample of community-dwelling knee osteoarthritis patients. J. Clin. Rheumatol. 20, 261–267. doi: 10.1097/RHU.0000000000000123
Smeets, R. J., Severens, J. L., Beelen, S., Vlaeyen, J. W., and Knottnerus, J. A. (2009). More is not always better: cost-effectiveness analysis of combined, single behavioral and single physical rehabilitation programs for chronic low back pain. Eur. J. Pain 13, 71–81. doi: 10.1016/j.ejpain.2008.02.008
Smith, B. E., Hendrick, P., Bateman, M., Moffatt, F., Rathleff, M. S., Selfe, J., et al. (2019). A loaded self-managed exercise programme for patellofemoral pain: a mixed methods feasibility study. BMC Musculoskelet. Disord. 20, 129. doi: 10.1186/s12891-019-2516-1
Smith, B. E., Littlewood, C., and May, S. (2014). An update of stabilisation exercises for low back pain: a systematic review with meta-analysis. BMC Musculoskelet. Disord. 15, 416. doi: 10.1186/1471-2474-15-416
Tagliaferri, S. D., Miller, C. T., Ford, J. J., Hahne, A. J., Main, L. C., Rantalainen, T., et al. (2020). randomized trial of general strength and conditioning versus motor control and manual therapy for chronic low back pain on physical and self-report outcomes. J. Clin. Med. 9, 1726. doi: 10.3390/jcm9061726
Takacs, J., Krowchuk, N. M., Garland, S. J., Carpenter, M. G., and Hunt, M. A. (2017). Dynamic balance training improves physical function in individuals with knee osteoarthritis: a pilot randomized controlled trial. Arch. Phys. Med. Rehabil. 98, 1586–1593. doi: 10.1016/j.apmr.2017.01.029
Tejera, D. M., Beltran-Alacreu, H., Cano-de-la-Cuerda, R., Leon Hernández, J. V., Martín-Pintado-Zugasti, A., Calvo-Lobo, C., et al. (2020). Effects of virtual reality versus exercise on pain, functional, somatosensory and psychosocial outcomes in patients with non-specific chronic neck pain: a randomized clinical trial. Int. J. Environ. Res. Public Health 17, 5950. doi: 10.3390/ijerph17165950
Tkachuk, G. A., and Harris, C. A. (2012). Psychometric properties of the Tampa Scale for Kinesiophobia-11 (TSK-11). J. Pain 13, 970–977. doi: 10.1016/j.jpain.2012.07.001
Urquhart, D. M., Phyomaung, P. P., Dubowitz, J., Fernando, S., Wluka, A. E., Raajmaakers, P., et al. (2015). Are cognitive and behavioural factors associated with knee pain? A systematic review. Semin. Arthritis. Rheum. 44, 445–455. doi: 10.1016/j.semarthrit.2014.07.005
Vihstadt, C., Maiers, M., Westrom, K., Bronfort, G., Evans, R., Hartvigsen, J., et al. (2014). Short term treatment versus long term management of neck and back disability in older adults utilizing spinal manipulative therapy and supervised exercise: a parallel-group randomized clinical trial evaluating relative effectiveness and harms. Chiropr. Man. Therap. 22, 26. doi: 10.1186/s12998-014-0026-7
Vincent, H., Seay, A., Montero, C., and Vincent, K. (2013). Outpatient rehabilitation outcomes in obese patients with orthopedic conditions. Eur. J. Phys. Rehabil. Med. 49, 419–429.
Weissenfels, A., Wirtz, N., Dörmann, U., Kleinöder, H., Donath, L., Kohl, M., et al. (2019). Comparison of whole-body electromyostimulation versus recognized back-strengthening exercise training on chronic nonspecific low back pain: A randomized controlled study. Biomed. Res. Int. 2019, 5745409. doi: 10.1155/2019/5745409
Wicksell, R. K., Olsson, G. L., and Hayes, S. C. (2010). Psychological flexibility as a mediator of improvement in acceptance and commitment therapy for patients with chronic pain following whiplash. Eur. J. Pain 14, 1059 e1051–1059.e1011. doi: 10.1016/j.ejpain.2010.05.001
Woby, S. R., Roach, N. K., Urmston, M., and Watson, P. J. (2005). Psychometric properties of the TSK-11: a shortened version of the Tampa Scale for Kinesiophobia. Pain 117, 137–144. doi: 10.1016/j.pain.2005.05.029
Xiang, L., Mei, Q., Wang, A., Shim, V., Fernandez, J., and Gu, Y. (2022). Evaluating function in the hallux valgus foot following a 12-week minimalist footwear intervention: A pilot computational analysis. J. Biomech.132, 110941. doi: 10.1016/j.jbiomech.2022.110941
Xu, D., Quan, W., Zhou, H., Sun, D., Baker, J. S., and Gu, Y. (2022). Explaining the differences of gait patterns between high and low-mileage runners with machine learning. Sci. Rep.12, 2981. doi: 10.1038/s41598-022-07054-1
Xu, Y., Song, Y., Sun, D., Fekete, G., and Gu, Y. (2020). Effect of multi-modal therapies for kinesiophobia caused by musculoskeletal disorders: a systematic review and meta-analysis. Int. J. Environ. Res. Public Health 17, 9439. doi: 10.3390/ijerph17249439
Yilmaz Yelvar, G. D., Çirak, Y., Dalkilin,ç, M., Parlak Demir, Y., Guner, Z., and Boydak, A. (2017). Is physiotherapy integrated virtual walking effective on pain, function, and kinesiophobia in patients with non-specific low-back pain? Randomised controlled trial. Eur. Spine J. 26, 538–545. doi: 10.1007/s00586-016-4892-7
Zdziarski, L. A., Wasser, J. G., and Vincent, H. K. (2015). Chronic pain management in the obese patient: a focused review of key challenges and potential exercise solutions. J. Pain. Res. 8, 63–77. doi: 10.2147/JPR.S55360
Zdziarski-Horodyski, L., Vasilopoulos, T., Horodyski, M., Hagen, J. E., Sadasivan, K. S., Sharififar, S., et al. (2020). Can an integrative care approach improve physical function trajectories after orthopaedic trauma? A randomized controlled trial. Clin. Orthop. Relat. Res. 478, 792–804. doi: 10.1097/CORR.0000000000001140
Keywords: kinesiophobia, musculoskeletal pain, network meta-analysis, systematic review, non-surgical
Citation: Huang J, Xu Y, Xuan R, Baker JS and Gu Y (2022) A Mixed Comparison of Interventions for Kinesiophobia in Individuals With Musculoskeletal Pain: Systematic Review and Network Meta-Analysis. Front. Psychol. 13:886015. doi: 10.3389/fpsyg.2022.886015
Received: 02 March 2022; Accepted: 30 May 2022;
Published: 29 June 2022.
Edited by:
Julia Maria D'Andréa Greve, University of São Paulo, BrazilReviewed by:
Mitchell Selhorst, Nationwide Children's Hospital, United StatesAlicia Fernandez-Fernandez, Nova Southeastern University, United States
Copyright © 2022 Huang, Xu, Xuan, Baker and Gu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rongrong Xuan, fyxuanrongrong@nbu.edu.cn; Yaodong Gu, guyaodong@hotmail.com
 Jialu Huang
Jialu Huang Yining Xu
Yining Xu Rongrong Xuan
Rongrong Xuan Julien S. Baker
Julien S. Baker Yaodong Gu
Yaodong Gu