Abstract
Ischemic stroke involves numerous and complex pathophysiological mechanisms including blood flow reduction, ionic exchanges, spreading depressions and cell death through necrosis or apoptosis. We used a mathematical model based on these phenomena to study the influences of intensity and duration of ischemia on the final size of the infarcted area. This model relies on a set of ordinary and partial differential equations. After a sensibility study, the model was used to carry out in silico experiments in various ischemic conditions. The simulation results show that the proportion of apoptotic cells increases when the intensity of ischemia decreases, which contributes to the model validation. The simulation results also show that the influence of ischemia duration on the infarct size is more complicated. They suggest that reperfusion is beneficial when performed in the early stroke but may be either inefficacious or even deleterious when performed later after the stroke onset. This aggravation could be explained by the depolarisation waves which might continue to spread ischemic damage and by the speeding up of the apoptotic process leading to cell death. The effect of reperfusion on cell death through these two phenomena needs to be further studied in order to develop new therapeutic strategies for stroke patients.



Similar content being viewed by others
References
Aitken PG, Jing J, Young J, Friedman A, Somjen GG (1991) Spreading depression in human hippocampal tissue in vitro. Third IBRO Congr. Montreal Abstr., 329
Back T, Hirsch JG, Szabo K, Gass A (2000) Failure to demonstrate Peri-infarct depolarizations by repetitive MR diffusion imaging in acute human stroke. Stroke 31:2901–2906
Barber PA, Auer RN, Buchan AM, Sutherland GR (2001) Understanding and managing ischemic stroke. Can J Physiol Pharmacol 79:283–296
Brouns R, De Deyn PP (2009) The complexity of neurobiological processes in acute ischemic stroke. Clin Neurol Neurosurg 111(6):483–495
Busch E, Gyngell ML, Eis M, Hoehn-Berlage M, Hossmann KA (1996) Potassium-induced cortical spreading depressions during focal cerebral ischemia in rats: contribution to lesion growth assessed by diffusion-weighted NMR and biochemical imaging. J Cereb Flow Metab 16:1090–1099
Chan PH (2002) Cerebrovascular disease 22nd princeton conference. Cambridge University Press, Cambridge
Chapuisat G (2007) Discussion of a simple model of spreading depression. ESAIM Proc 18:87–98
Chapuisat G, Dronne MA, Grenier E, Hommel M, Gilquin H, Boissel JP (2008) A global phenomenological model of ischemic stroke with stress on spreading depressions. Prog Biophys Mol Biol 97(1):4–27
Cheng YD, Al-Khoury L, Zivin JA (2004) Neuroprotection for ischemic stroke: two decades of success and failure. NeuroRx 1:36–45
De Keyser J, Sulter G, Luiten PG (1999) Clinical trials with neuroprotective drugs in acute ischaemic stroke: are we doing the right thing? Trends Neurosci 22:535–540
Devuyst G, Bogousslavsky J (2001) Recent progress in drug treatment for acute ischemic stroke. Cerebrovasc Dis 11(Suppl 1):71–79
Dirnagl U, Iadecola C, Moskowitz MA (1999) Pathobiology of ischaemic stroke: an integrated view. Trends Neurosci 22:391–397
Dohmen C, Sakowitz OW, Fabricius M, Bosche B, Reithmeier T, Ernestus RI, Brinker G, Dreier JP, Woitzik J, Strong AJ, Graf R (2008) Spreading depolarizations occur in human ischemic stroke with high incidence. Ann Neurol 63(6):720–728
Doyle KP, Simon RP, Stenzel-Poore MP (2008) Mechanisms of ischemic brain damage. Neuropharmacol 55(3):310–318
Dronne MA, Boissel JP, Grenier E (2006) A mathematical model of ion movements in grey matter during a stroke. J Theor Biol 240(4):599–615
Dronne MA, Grenier E, Dumont T, Hommel M, Boissel JP (2007) Role of astrocytes in grey matter during stroke: a modelling approach. Brain Res 23:231–242
Durukan A, Tatlisumak T (2007) Acute ischemic stroke: overview of major experimental rodent models, pathophysiology, and therapy of focal cerebral ischemia. Pharmacol Biochem Behav 87(1):179–197
Furlan AJ, Katzan IL, Caplan LR (2003) Thrombolytic therapy in acute ischemic stroke. Curr Treat Options Cardiovasc Med 5:171–180
Gorji A, Scheller D, Straub H, Tegtmeier F, Kohling R, Hohling JM, Tuxhorn I, Ebner A, Wolf P, Werner Panneck H, Oppel F, Speckmann EJ (2001) Spreading depression in human neocortical slices. Brain Res 906(1–2):74–83
Grenier E, Dronne MA, Descombes S, Gilquin H, Jaillard A, Hommel M, Boissel JP (2008) A numerical study of the blocking of migraine by Rolando sulcus. Prog Biophys Mol Biol 97(1):54–59
Heinemann U, Lux HD (1977) Ceiling of stimulus induced rises in extracellular potassium concentration in the cerebral cortex of cat. Brain Res 120(2):231–249
Hossmann KA (2006) Pathophysiology and therapy of experimental stroke. Cell Mol Neurobiol 26(7–8):1057–1083
Kato H, Kogure K (1999) Biochemical and molecular characteristics of the brain with developing cerebral infarction. Cell Mol Neurobiol 19:93–108
Koroshetz WJ, Moskowitz MA (1996) Emerging treatments for stroke in humans. Trends Pharmacol Sci 17:227–233
Kyoung Shin H, Dunn AK, Jones PB, Boas DA, Moskowitz MA, Ayata C (2006) J Cereb Blood Flow Metab 26:1018–1030
Lassen NA (1990) Pathophysiology of brain ischemia as it relates to the therapy of acute ischemic stroke. Clin Neuropharmacol 13(Suppl 3):S1–S8
Lauritzen M, Hansen AJ (1992) The effect of glutamate receptor blockade on anoxic depolarization and cortical spreading depression. J Cereb Blood Flow Metab 12:223–229
Lauritzen M, Skyhoj Olsen T, Lassen NA, Paulson OB (1983) Changes in regional cerebral blood flow during the course of classic migraine attacks. Ann Neurol 13:633–641
Lees KR (2000) Neuroprotection. Br Med Bull 56:401–412
Liebeskind DS, Kasner SE (2001) Neuroprotection for ischaemic stroke: an unattainable goal? CNS Drugs 15:165–174
Martinez-Vila E, Sieira PI (2001) Current status and perspectives of neuroprotection in ischemic stroke treatment. Cerebrovasc Dis 11(Suppl 1):60–70
Mayevsky A, Doron A, Manor T, Meilin S, Zarchin N, Ouaknine GE (1996) Cortical spreading depression recorded from the human brain using a multiparametric monitoring system. Brain Res 740:268–274
McCord LM (1985) Oxygen-derived free radicals in postichemic tissue injury. N Engl J Med 312:159–163
McLachlan RS, Girvin JP (1994) Spreading depression of Leao in rodent and human cortex. Brain Res 666(1):133–136
Mehta SL, Manhas N, Raghubir R (2007) Molecular targets in cerebral ischemia for developing novel therapeutics. Brain Res Rev 54(1):34–66
Mies G, Iijima T, Hossman KA (1993) Correlation between peri-infarct DC shifts and ischaemic neuronal damage in rat. Neuroreport 4:709–711
Molina CA, Alvarez-Sabín J (2009) Recanalization and reperfusion therapies for acute ischemic stroke. Cerebrovasc Dis 27(Suppl 1):162–167
Mongin AA (2007) Disruption of ionic and cell volume homeostasis in cerebral ischemia: the perfect storm. Pathophysiol 14(3–4):183–193
Nedergaard M, Hansen AJ (1988) Spreading depression is not associated with neuronal injury in the normal brain. Brain Res 449:395–398
O’Collins VE, Macleod MR, Donnan GA, Horky LL, van der Worp BH, Howells DW (2006) 1,026 experimental treatments in acute stroke. Ann Neurol 59(3):467–477
Obeidat AS, Jarvis CR, Andrew RD (2000) Glutamate does not mediate acute neuronal damage after spreading depression induced by O2/glucose deprivation in the hippocampal slice. J Cereb Blood Flow Metab 20(2):412–422
Phan TG, Wright PM, Markus R, Howells DW, Davis SM, Donnan GA (2002) Salvaging the ischaemic penumbra: more than just reperfusion? Clin Exp Pharmacol Physiol 29:1–10
Rogers SJ, Sherman DG (1993) Pathophysiology and treatment of acute ischemic stroke. Clin Pharm 12:359–376
Somjen GG (2004) Ions in the brain: normal function, seizures, and stroke. Oxford university press, Oxford
Sramka M, Brozek G, Bures J, Nadvornık P (1977) Functional ablation by spreading depression: possible use in human stereptactic surgery. Appl Neurophysiol 40:48–61
Strong AJ, Fabricius M, Boutelle MG, Hibbins SJ, Hopwood SE, Jones R, Parkin MC, Lauritzen M (2002) Spreading and synchronous depressions of cortical activity in acutely injured human brain. Stroke 33(12):2738–2743
Taoufik E, Probert L (2008) Ischemic neuronal damage. Curr Pharm Des 14(33):3565–3573
Wahlgren NG, Ahmed N (2004) Neuroprotection in cerebral ischaemia: facts and fancies—the need for new approaches. Cerebrovasc Dis 17(Suppl 1):153–166
Zweifler RM, Brody ML, Graves GC, Drinkard R, Cunningham S, Rothrock JF (1998) Intravenous t-PA for acute ischemic stroke: therapeutic yield of a stroke code system. Neurology 50:501–503
Acknowledgments
This work was supported by the French Ministry of Research (ACI “AVC-iSi”, project 02TS041).
Author information
Authors and Affiliations
Corresponding author
Appendix A: Equations of the Model
Appendix A: Equations of the Model
1.1 A.1 List of the Variables
In the following equations, t refers to the time and x to the place in the brain. Hence x is a vector of dimension 1, 2 or 3, depending on the dimension of the brain that we are considering. For example, in this paper we are working on a section of the brain, hence x = (x1, x2) is a two-coordinates vector.
- η(t):
-
fraction of blood flow in the occluded vessel during the stroke in function of time t
- BFlow (t, x):
-
proportion of blood flow that irrigates the cells at location x and time t
- BFlow vessel (x):
-
physiological proportion of blood flow carried to the cells at location x by the vessel that will be occluded
- BFlow others (x):
-
physiological proportion of blood flow carried to the cells at location x by the vessels that will remain sane
- OEF (t, x):
-
oxygen extraction factor at time t in the cells at location x
- OEF∞ (BF):
-
stationary value of the oxygen extraction factor for cells that receive a blood flow BF
- Eav (t, x):
-
available energy at time t in the cells at location x
- Emeta, used (t, x):
-
energy used to maintain life at time t in the cells at location x
- Ehomeo, used (t, x):
-
energy used to maintain homeostasis at time t in the cells at location x
- ESD, used (t, x):
-
energy used to recover from spreading depressions at time t in the cells at location x
- Eact, used (t, x):
-
energy used to have an electrical activity at time t in the cells at location x
- Erem (t, x):
-
remainder energy at time t in the cells at location x
- Caa (t, x):
-
astrocytic calcium concentration difference between the cells at location x and time t and the resting state
- Can (t, x):
-
neuronal calcium concentration difference between the cells at location x and time t and the resting state
- Ke (t, x):
-
extracellular potassium concentration difference between time t and location x and the resting state
- Cap (t, x):
-
capacity of the cells at location x to recover from SD at time t
- R (t, x):
-
strength of the recovery mechanism from spreading depression for the cells at location x and time t
- \( \Uptheta (t,{\text{x}}) \) :
-
state of the cells at location x and time t
- Repair (t, x):
-
ability to repair of the cells at location x and time t
- Damage (t, x):
-
damage to the cells at location x and time t
- A (t, x):
-
progress of the apoptosis process at time t in the cells at location x
1.2 A.2 List of the Equations
The significances of the parameters used in the following equations are given in section A.3.
1.2.1 A.2.1 Blood Flow
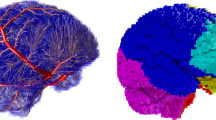
By definition of BFlowvessel and BFlowothers, we have: BFlowvessel (x) + BFlowothers (x) = 1.(see Fig. 1 for a representation of BFlowothers)
During the stroke, the blood flow at point x and time t is given by:
with \( {{\upeta}}(t) = {\kern 1pt} \,\left\{ {\begin{array}{*{20}c} {\eta_{0} \quad {\text{if}}\; t \le {\text{T}}_{\text{isch}} } \\ {1\quad {\text{if}}\; t > {\text{T}}_{\text{isch}} } \\ \end{array} } \right. \)
1.2.2 A.2.2 Oxygen Absorption
The equations that govern the oxygen extraction factor (OEF) are:
1.2.3 A.2.3 Energy
The available energy for a cell is assumed to be proportional to the oxygen extracted from blood:
This available energy is used for the four main tasks: maintaining metabolism, maintaining homeostasis, recovering from spreading depressions and creating an electrical activity:
with \( {\text{E}}_{\text{need}} = {\text{E}}_{\text{meta}} + {\text{E}}_{\text{homeo}} + {\text{E}}_{\text{SD}} + {\text{E}}_{\text{act}} \)
The remaining energy is used for other secondary tasks:
So we have:
1.2.4 A.2.4 Ionic Exchanges
For simplicity reasons, the variables t and x have not been written in the following equations.We recall the definition of the Laplacian \( \Updelta = \sum\nolimits_{k = 1}^{n} {{\frac{{\partial^{2} }}{{\partial x_{k}^{2} }}}} \) where n is the dimension of the space. We also define 1{A>a} = 1 if A > a and 1{A>a} = 0 if A ≤ a.
The ionic exchanges between intra- and extracellular spaces are governed by the following equations:
The recovery mechanisms (from spreading depressions) are governed by the following equations:
1.2.5 A.2.5 Cell Death
In order to determine if a cell survives or not, we quantify the state of a cell as follows:
Repair quantifies the cell ability to “repair”:
Damage quantifies the cell damage due to the excess of intracellular calcium:
If \( \Uptheta (t,{\text{x}}) > \Uptheta_{\text{apop}} \), the apoptosis has not begun: A = 0. If \( \Uptheta (t,{\text{x}}) \le \Uptheta_{\text{apop}} \), the apoptosis process progresses:
Conclusion:
-
If \( \Uptheta \) stays above \( \Uptheta_{\text{apop}} \), the cells are alive.
-
If A passes over Aapop before \( \Uptheta \) passes above \( \Uptheta_{\text{nec}} \), the cells are dead by apoptosis.
-
If \( \Uptheta \) passes above \( \Uptheta_{\text{nec}} \) before A passes over Aapop, the cells are dead by necrosis.
1.3 A.3 List of the Parameters
Rights and permissions
About this article
Cite this article
Chapuisat, G., Dronne, MA., Grenier, E. et al. In Silico Study of the Influence of Intensity and Duration of Blood Flow Reduction on Cell Death Through Necrosis or Apoptosis During Acute Ischemic Stroke. Acta Biotheor 58, 171–190 (2010). https://doi.org/10.1007/s10441-010-9100-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10441-010-9100-2