Abstract
Medical resource allocation is a controversial topic, because in the end it prioritises some peoples’ medical problems over those of others. This is less controversial when there is a clear clinical reason for such a prioritisation, but when such a reason is not available people might perceive it as deeming certain individuals more important than others. This article looks at the role of social utility in medical resource allocation, in a situation where the clinical outcome would be identical if either person received the treatment. This situation is explored with a focus on the United Kingdom, but its conclusions have wider applications to any system where healthcare is tax-payer funded. The article proposes an experience adjusted life years system, and discusses its strengths and weaknesses.
Similar content being viewed by others
Introduction
This work examines the issue of medical resource allocation to patients in a clinically identical state. It introduces the concept of medical resource allocation and the controversies associated with such allocations, especially those related to the age of the patient. It also scrutinises the concept of quality adjusted life years (QALY) and introduces the concept of experience adjusted life years (EALY). The rest of the work examines the use of EALY under different circumstances, highlighting its strengths and weaknesses.
This work is based primarily on the situation present in the United Kingdom (UK): values held by the National Health Service (NHS) and the National Institute for Health and Care Excellence (NICE), as well as other commentaries on British societal values. For a wider discussion on European health care resource allocation, as well as on how it contrasts with the situation in the UK and the USA (see e.g.: Jakubowski and Busse 1998; Hurst et al. 2007; Teutsch and Rechel 2012; Nagy 2015).
Though EALY is, in essence, a utilitarian concept, it is not the aim of this paper to promote such a mode of bioethical reasoning. Rather, it aims to show the possible uses of such a system and the downfalls associated with it. In making that point, this paper hopes to encourage decision-makers to critically re-evaluate how they manage medical resources, especially in emergency situations, and provide a tool for such decision making.
Medical resource allocation
Medical resource allocation is a two-tier problem (Luchetti 2013). The macro scale is managed by politicians and high-level managers deciding which hospitals and wards are given what resources. The micro-scale is where clinicians decide which patients can receive what treatments. There are limits on medical resources (Maynard 1996; Hurst et al. 2007; Neuberger 2012; Luchetti 2013), be they therapeutic agents, diagnostic equipment, bed space or clinician time. Though the allocation of such resources could be random/via a lottery (Childress 1970), such a stance is wasteful, as some patients might benefit from them more than others (Persad et al. 2009; Neuberger 2012). Both tiers face similar difficulties: to be fair, just and efficient, and how to define these parameters. It is doubtful that calculating patient benefit in a way that would gain widespread acceptance, without subjectivity or ambiguity, is possible (ATS Bioethics Task Force 1997), or that fairness can be achieved without sacrificing efficiency (Maynard 1996).
In emergency cases allocating resources efficiently can mean the difference between life and death. To this end, various forms of triage have been developed. These vary from protocols categorising people into tiers during mass casualty events, the grading of ambulance calls, and the judgement of a triage nurse. These patient assessment systems are designed to allocate resources to those who need them most and will gain the most from them, and there is major agreement that this should be the primary criteria for such decisions (Childress 1970; ATS Bioethics Task Force 1997; Jones et al. 2011; Ventilator Document Workgroup 2011). These systems are, nevertheless, not designed to arbiter allocations between patients who are in a clinically identical state and arrive for treatment at the same time. However, such situations are plausible, especially in conditions of sever scarcity where allocation models are less applicable (ATS Bioethics Task Force 1997), and still a subject of debate (Burkle 2002; Committee on Guidance for Establishing Standards of Care for Use in Disaster Situations 2009; White et al. 2009).
When resolving complex allocation problems, multivariable systems need to be utilised to account for all the values deemed to be important (Persad et al. 2009). They are, nevertheless, hard to execute, especially in emergency cases (White et al. 2009). This will stop being a practical obstacle with the digitalisation and integration of patient information with public data, and the development of more efficient information systems. Successful application of EALY’s would rely on such an information system.
NICE’s use of QALY
NICE uses QALY in its decision-making process (Rawlins and Culyer 2004; Jones et al. 2011), and it is a body from which the NHS takes its guidelines. QALY factors in the amount of years gained from a treatment, but puts less weight on years lived by people suffering from various disabilities—it measures the amount of life to be lived, rather than the number of years lived. NICE puts no weight on the age (unless it affects clinical prognosis), sex or ethnicity of the persons treated—all quality adjusted years are equivalent (Rawlins and Culyer 2004). Further, NICE refuses to take account of any personal ‘deservedness’ of the patient (Rawlins and Culyer 2004), in which it is not alone (Childress 1970; Rawlins and Culyer 2004; Sprung et al. 2013).
If NICE decided to use social worth as a factor, this might have affected societal cohesion, caused inter-class struggle, but also ultimately affected how people view one another and for what they value each other, hence forsaking public ethics considerations (White et al. 2009). Nevertheless, quality of life is itself a highly speculative and arbitrary factor that has been criticised itself (Jones et al. 2011), e.g. for discriminating against those with disabilities. Yet, social worth, or rather specific aspects and interpretations of it,Footnote 1 can be measured in many more objective ways than QALY, e.g. through contribution to gross domestic product (GDP), and so can another factor generally ignored by NICE, but being generally a good predictor of QALY, age. Hence, the following sections will evaluate age and social worth considerations in resource allocation decisions.
Fair innings and resource allocation
In situations of equal clinical need/outcome the number of years saved is one of the few leftover criteria that might be available to help resolve an allocation conflict. This criterion seems both utilitarian and egalitarian, but it is closely related to the patients’ age, and hence might lead to the preferential treatment of the young. Schemes of medical resource allocation based majorly on age have been known under various names: fair innings, life cycle principle, and intergenerational equality (White et al. 2009). A brief description of fair innings, based on Harris’ (2001) definition, is:
Seventy years is a fair share of life. We should distribute medical resources to maximise the number of people living until 70. Treating people older than 70 is permissible if it does not deprive a person below the age of 70 of any necessary medical treatment.
The fair innings argument is therefore not based on hate of the elderly, but on a notion that there is some fairness in letting the young live to an age already achieved by the aged (Persad et al. 2009). Lilford highlights that the key fair innings assumption of “other things being equal” favours the young, and allows for swift clinical decision making (Lilford 1995 responding to; Rivlin 1995) when a resource allocation conflict occurs. Rivlin’s rebuttal, showed that such reasoning does not survive philosophical scrutiny, by presenting six major problems with the fair innings argument (Rivlin 2000), which revolve around the problems with defining the concepts of fair and share in the context of life:
-
1.
What is a fair share of life?—It is hard to estimate between whom and how life is being shared, or even predict an individual’s life span to determine how much of it is potentially being shared. Further, one cannot give a share of one’s life, at most sacrifice it for someone else.
-
2.
What is a fair share of resources?—in the case of the NHS, the government might provide different recourses to the NHS and the public at different points of an individual’s life span. Further, what exactly should be counted as resources (equipment, buildings, individuals’ salaries, their skillsets)?
-
3.
Using fairness only with reference to the length of life—fairness can relate to other things, be it quality of life, or injustices that one has to suffer (e.g. an old person being struck by a young driver).
-
4.
Problems with the all “other things being equal” argument—it is almost impossible for all other things to be equal in a resource allocation problem involving two patients.
-
5.
Difference between fair and unfortunate—there is no objective reason for there being a length of life to which everyone should have a claim to, hence there is no fair age to live, some people are just more fortunate than others and live longer.
-
6.
Discrepancy between emotional descriptions of deaths of young and old people—it is not clear that the death of e.g. a young ruffian should be regarded as more tragic than that of an old person who was engaged in community work.
Age itself is a factor with at least two edges, as it is hard not to appreciate the experience of the old and the hopes of the young, the present grandparent and the future parent, a true child of a community and the new-born child of a young couple. A more senior age implies both less life years to save, but also more experience to preserve. Therefore, this article will further evaluate social worth as a potential factor in allocation decisions, which makes all other things never equal, but also has its flaws.
EALY
This section will introduce the concept of EALY as an alternative to QALY. QALY was certainly not primarily developed as a tool for emergency micro allocations, hence it does not consider certain characteristics that might be useful in situations of radical scarcity (where standard triage protocols might also not possess enough power to do their job). EALY tries to remedy this by analysing some of the values of the NHS, the dominant British healthcare provider, which is taxpayer funded.
The NHS states that it “provides a comprehensive service available to all”, “[a]ccess to NHS services is based on clinical need, not an individual’s ability to pay”, and that “[t]he NHS is committed to providing best value for taxpayers’ money and the most effective, fair and sustainable use of finite resources” (NHS Choices 2015). Although these principles refute prioritising patients based on their ability to pay, they muddle whether priority treatment of some individuals provides the most effective use of taxpayers’ money. People with skills of high demand, and those offering employment opportunities to others, might be more worth taxpayers’ health money, since they can then contribute to increasing the pool of said “finite resources” and hence are more “sustainable”. This is especially true when treating health professionals in times of medical emergency, as they can then contribute to alleviating that emergency (Pesik et al. 2001). Similarly treating care-givers might be more important for society than independent people (Rescher 1969). It remains uncertain how this would relate to the criterion of “fair[ness]”, but at least the treatment would be still primarily prioritised based on need.
Two objections can be raised here. Firstly, that the sustainability of a healthcare system is an internal issue, divorced from the wider economic context. Furthermore, a country with a low GDP can still devote a large percentage of it to healthcare. As much as these are true to some extent, the amount of money a government can devote to healthcare is, nevertheless, somewhat related to the pool of money it has collected through such means as taxation. Secondly, it could be objected that this is not the way the NHS views the principle of “sustainability”, for it relates to how the NHS spends money on services, rather than on which service users does it spend it. As such, the analysis in the previous paragraph should be treated as an alternative interpretation of sustainability. Nevertheless, such an interpretation might become more relevant when resources are very scarce, as will be demonstrated in a later section discussing the potential UK response to a war scale emergency.
The need for fair resource distribution (ATS Bioethics Task Force 1997; Persad et al. 2009) does not necessarily imply a random distribution, but only precludes undue favouritism (Rescher 1969), and requires transparency and consistency, so as to prevent social unrest (Committee on Guidance for Establishing Standards of Care for Use in Disaster Situations 2009; Silva et al. 2012). Rescher argued that “utility requires reference of services to be rendered and justice calls for a recognition of services that have been rendered”Footnote 2 (Rescher 1969). It is on such assumptions of fairness, utility and justice that EALY is based upon. Additionally, a system based on such assumptions might motivate people to live more virtuously, though it is somewhat unclear what such virtuousness should entail (Sanders and Dukeminier 1967).
Though selecting criteria for estimating social worth is extremely difficult (Childress 1970), the skillsetFootnote 3 of a population is an important asset. Along with natural resources it is a means of establishing a degree of autonomy and economic prosperity, and hence beneficial for the majority of the population. Furthermore, education, health and general prosperity are positively correlated (Higgins et al. 2008), hence, factoring in skill does not seem to depart far from factoring in quality of life, while avoiding its subjectivity. Finally, as discussed earlier, older people might have skills and life experience important for the young, and this is something not considered by QALY or the fair innings argument: that the innings of the young are to some degree connected with the lives of the old, and the life quality of the less skilled with this of the more skilled.
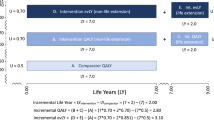
EALY is best illustrated in graphical terms (Fig. 1). These graphs assume the length of life of an individual to be 81 years and that a skilled worker is worth 1.74 of an unskilled worker based on salary differences between A-level and university-level graduates (Office for National Statistics 2016). To factor in experience of the person, their worth will increase every year by (an arbitrary) 0.30% from the age of 18 for unskilled workers and 0.33% from the age of 22 for skilled workers (assuming that skilled workers engage in more continuous professional development) and both groups suffer a single cut of 50% at the retirement age of 65.
Depiction of the relationship of EALY to age, when EALY is estimated on the basis of formal education. a Shows the EALY contribution of an individual at a given age. b Shows the total past EALY contribution of an individual by a given age. c Shows the amount of EALY gained by society when an individual’s life is saved at a given age. The dotted line represents a high skilled individual; the solid line represents a low skilled individual
This is not to assume that formal education is the only way to gain a valuable skillset, but it is a convenient way of modelling the skilfulness of an individual. Other factors or tests, including multifactorial calculations, could be used to determine a more appropriate starting point e.g. via a combination of internships, education and aptitude tests. Some traits like empathy and the impact someone has on other people’s wellbeing are clearly harder to assess. Nevertheless, the model does take into account the experience gained with years which accounts for the impact of general life experience. Again, this might not hold true for a single individual, as people might experience significant events in their lives that allow them to gain more experience and skills in a short period of time (e.g. when dealing with a significant family or work event) and there are factors that can detract from it, such as some medical events (e.g. traumatic brain injury). Henceforth, the particular assumptions made in the model used in Fig. 1 should be treated as a way of demonstrating the general assumptions made by EALY. Further, the aim of Fig. 1 is to model the population as a whole, rather than any one particular individual. As discussed later, this model could be modified to suit the profile and current need of a population with respect to EALY assessment.
From Fig. 1 several important observations can be made. First, it can be noted from panel A that though the unskilled worker gets a head start, by the time of graduation the skilled worker’s yearly EALY is already much higher. Further, panel B shows that by the age of 29 the past contributions of the skilled worker exceed those of the unskilled worker. Nevertheless, the implications for medical resource allocations are clearest in panel C. There it is observable that the EALY benefit to society is similar when saving a 19-year-old low skill worker as is saving a 41-year-old high skill worker, as they will be able to contribute the same amount of skill and experienced over their remaining lifetimes. Or to use Harris’ cut off age of 70 (Harris 2001), a 70-year-old high skill worker could only be out-prioritised by a pre-retirement low skill worker. The fair innings argument, at least in its simplest form, does not hold under such a utilitarian analysis, for some older people might have expertise that is more valuable to society than that which the young can offer.
If QALY is a measure of the amount of life saved, then EALY is a measure of amount of service to society saved. What remains to be determined now is what effect on society would EALY elicit—whether it would be an acceptable tool for most people. Those that argue for the equal worth of every life (Childress 1970) under any circumstances, might only accepted one conclusion from Fig. 1a. That an 81 with a lot of life experience is worth basically as much as a fresh sixth form graduate with no experience.
Use of EALY in a national emergency
This paper is set in the context of an allocation decision having to be made when clinical outcome between two patients would be identical, but only one can be treated. Therefore, a reasonable set of circumstances for the evaluation of EALY is the context of a local or national emergency, be it something of the scale of the Paris terrorist attacks (Hirsch et al. 2015), a flue pandemic (Frolic et al. 2009), or any terrorist attack occurring in a highly crowded area, like during the Boston Marathon or the Manchester concert (Osterweil 2015; Palazzo and Allen 2017). These are situations where many casualties might present at the same time in a similar condition, requiring urgent care, i.e. when demand might exceed the resources available.
After analysing two important documents on the British prospective response to a war scale emergency (Campbell 1982; British Medical Association 1983), Burkle highlights that the UK government would in certain circumstances write off whole cities and even refuse the provision of simple comfort measures to people (Burkle 2002). Such radical situations seem to require prioritisation of a nation’s need for recovery and stability of government that might require ruthless triage (Campbell 1982). This extreme sacrifice would result in great damage to British culture and society, whose preservation is also a governmental task (Campbell 1982).
Using EALY in emergency situations would help preserve “mission-critical resource[s]” (Pesik et al. 2001)—not dissimilar to how health and social workers are privileged with respect to vaccinations (NHS Choices 2016). The people whose treatment is being prioritised are not treated better because they are deemed to be more worthy as human beings, but because the wellbeing of other people depends on them. Use of EALY in emergencies could save more lives on both short and long term timescales, and hence be accepted by the wider society. Under these conditions EALY could be said to be “providing best value for taxpayers” and sustainable use of finite resources” (NHS Choices 2015).
Strengths and weaknesses of EALY
EALY’s main strength is that it provides a clear guide on how to allocate resources between two patients who have identical clinical needs. EALY can be consistently and transparently applied between cases. Further on, the criteria used for EALY, at least in emergency cases, seem to be arguably consistent with British values, and can promote societal resilience. Further, it avoids the use of subjective measures of quality of life, and therefore EALY mitigates, to some extent, problems associated with QALY, as at least some disabilities would not affect EALY scores (e.g. in those whose disability does not majorly affect their work). Finally, the way how EALY is scored could be adjusted to fit the emergency with which a society is currently dealing (e.g. by adjusting sores for specific types of experience).
The main weaknesses of the EALY approach are the scope of its applicability and the possible reaction of the public to it, both these being somehow related to each other. This paper argued that using EALY might increase resilience, hence it is particularly useful in emergency situations, while otherwise it might promote elitism and instrumentalisation of human life. Similar criticisms are currently voiced within the wider British societal context (e.g. the Don’t Screen Us Out campaign 2017), and with respect to NICE’s use of QALY (e.g. Jones et al. 2011), and show that the government values disabled lives less. In some cases governmental policies have produced effects that are “[m]ore efficient than effective” (The Economist 2014). Use of EALY would not solve this problem, but possibly shift any discrimination from one group to another. It would shift the debate away from whether the old or the young are prioritized (Royal College of Peadiatrics and Child Health 2017; Kirkup 2013; Stewart 2013), and instead emphasise human instrumental value. Even if medical need remained the primary criterion for treatment, everyday use of EALY would remain susceptible to criticisms of elitism, of which the UK is still being accused of (Weale 2016; Medland 2017). In the past such social worth considerations did cause scandal, as exemplified by a certain kidney dialysis programme in the USA (Sanders and Dukeminier 1967). While in times of need citizens might accept that some individuals are more important for societal wellbeing, in times of peace they might not accept that those who are likely to be already better off should be even more better off. Surely people do not want to be just treated as a means of increasing the GDP.
It is noteworthy that utilitarian calculations are already used to some degree when allocating resources (e.g. lungs for transplantation) not necessarily to those who need them most, but to those who will potentially benefit the most from the procedure (e.g. non-obese non-smokers). Further, philosophers have already hypothetically used QALY in individual cases (Savulescu and Singer 2017). When clinical need nor patient arrival time can be used to discriminate between cases, short of throwing the hypothetical coin, some form of valuating patients is needed for an allocation decision to be made. Therefore, the problem faced by EALY will be faced by any allocation framework. As such, the key question is whether the assumptions underlying EALY are reasonable and acceptable to the wider population.
Instrumentalisation might not be tolerated when there is no need for an increase in resilience, and in such circumstances random allocationFootnote 4 might be preferable to mitigate any tension between the public and medical professionals. Nevertheless, a public consultation might reveal an acceptance of EALY in non-emergency situations, as long as clinical need prevails as the main criterion of medical resource allocation decisions. Use of EALY without the qualification of the primacy of treatment need will most certainly, and rightly, be rejected as elitist. Public debate about the way how conflicts in resource allocation should be resolved and about the value of efficiency in UK medical policies would help to clarify these issues.
Taking these strengths and weaknesses into account and in the absence of clear societal agreement to the contrary, EALY is best used within the limited context of emergency situations according to the flow diagram in Fig. 2. Though some might perceive EALY as a “‘least bad’ solution” (Lilford 1995) to what could be labelled as a complex problem of distributive justice, the use of EALY according to Fig. 2 provides an answer that promotes efficiency within reason in what is clearly an unusual emergency situationFootnote 5. As such EALY, can be a powerful decision-making tool, fit for a specific job. This job specificity is not an inherent weakness of EALY, but a consequence of the fact that not all circumstances are identical and hence might require a different method of evaluation.
Conclusion
This paper looked at medical resource allocation in a situation where treatment can only be given to one patient, when two patients are in a clinically identical situation. It discussed some of the values taken into account when allocation decisions are being made. Then it proposed EALY as a decision-making model.
EALY was shown to offer a transparent method, consistent with current British policy values, for resolving conflicts in resource allocation decisions when societal resilience needs to be maintained: in times of major emergencies, epidemics and war. In other situations, EALY might prove to be too elitist to merit its application, though a public debate about EALY’s application might prove its wider acceptance. As such, at the moment EALY should be treated as an allocation tool for a specific set of circumstances.
Additionally, EALY reasoning has revealed certain flaws in utilitarian considerations of age in the resource allocation debate, as well as mitigated some of the problems and limitations associated with QALY. Therefore, while not being a universal solution to all resource allocation problems, EALY offers a powerful decision-making tool for those having to make allocation decision in emergency cases.
Notes
There are many aspects of social worth that society might wish to include in allocation decisions, but which are hard to put into numbers. For example, the contribution of primary school teachers and entertainers towards society might not be best assessed by the income they have directly generated. Similarly, the contribution of those injured in the service of their country or community might be better understood through the inspiration they can generate in other people towards living virtuous and productive lives, rather than in their manual skillset or scholarly knowledge.
Emphasis mine.
How to exactly define a skillset is somewhat unclear and will be commented on later in the paper. In general, skillset should not denote just raw technical ability, but should also include soft skills and general life experience.
Subject to prior evaluation of clinical need and arrival time.
Here the language of Finnis (2011) has been employed, though no suggestion is made as to whether Finnis himself would agree with the reasonableness of EALY or the extraordinary nature of the circumstances surrounding its proposed use.
References
ATS Bioethics Task Force. 1997. Fair allocation of intensive care unit resources. American Journal of Respiratory and Critical Care Medicine 156: 1282–1301.
British Medical Association. 1983. The Medical Effects of Nuclear War: The Report of the British Medical Association’s Board of Science and Education. Chichester: Wiley.
Burkle, Frederick M. 2002. Mass casualty management of a large-scale bioterrorist event: An epidemiological approach that shapes triage decisions. Emergency Medicine Clinics of North America 20: 409–436. https://doi.org/10.1016/S0733-8627(01)00008-6.
Campbell, Duncan. 1982. War Plan UK: The Truth About Civil Defence in Britain. London: Burnett Books.
Childress, James F. 1970. Who shall live when not all can live? Soundings 53: 339–355.
Committee on Guidance for Establishing Standards of Care for Use in Disaster Situations. 2009. Guidance for Establishing Crisis Standards of Care for Use in Disaster Situations: A Letter Report. Washington, D.C.: National Academies Press.
Don’t Screen Us Out campaign. 2017. Don’t Screen Us Out campaign. Don’t Screen Us Out. http://dontscreenusout.org/. Accessed January 12, 2017.
Finnis, John. 2011. Natural Law and Natural Rights. 2 ed. New York: Oxford University Press.
Frolic, Andrea, Anna Kata, and Peter Kraus. 2009. Development of a critical care triage protocol for pandemic influenza: Integrating ethics, evidence and effectiveness. Healthcare Quarterly 12: 56–64.
Harris, John. 2001. The Value of Life: An Introduction to Medical Ethics. New York: Routledge.
Higgins, Claire, Teresa Lavin, and Owen Metcalfe. 2008. Health Impacts of Education: A Review. Edited by Institute of Public Health in Ireland. Dublin: Institute of Public Health in Ireland.
Hirsch, Martin, Pierre Carli, Rémy Nizard, Bruno Riou, Barouyr Baroudjian, Thierry Baubet and Vibol Chhor. 2015. The medical response to multisite terrorist attacks in Paris. The Lancet 386: 2535–2538. https://doi.org/10.1016/S0140-6736(15)01063-6.
Hurst, Samia A., Reidun Forde, Stella Reiter-Theil, Anne-Marie Slowther, Arnaud Perrier, Renzo Pegoraro, and Marion Danis. 2007. Physicians’ views on resource availability and equity in four European health care systems. BMC Health Services Research 7: 137. https://doi.org/10.1186/1472-6963-7-137.
Jakubowski, Elke, and Reinhard Busse. 1998. Health Care Systems in the EU: A Comparative Study. eds. Graham R. Chambers. Brussels: Eurpoean Parilament.
Jones, David, Ashley Albert, Beck, and Paul Gately. 2011. Healthcare Allocation and Justice: Applying Catholic Social Teaching. London: Catholic Truth Society.
Kirkup, James. Britain’s Forgotten Million Old People. The Telegraph, October 17, 2013.
Lilford, R. J. 1995. Flaws in agist arguments. Doctors need pragmatic strategies. BMJ: British Medical Journal 311: 752–753.
Luchetti, Marco. 2013. Intensive care resource allocation: When difficult choices have to be made. British Journal of Medical Practitioners 6: a633.
Maynard, Alan. 1996. Rationing health care: What use citizens’ juries and priority committees if principles of rationing remain implicit and confused? BMJ: British Medical Journal 313: 1499–1499.
Medland, Dina. A “Deeply Elitist Society”: U.K. Report Reveals Earnings Inequality by Social Background. Forbes. January 26, 2017.
Nagy, Balázs. 2015. Improving the Allocation of Health Care Resources in Poland. Geneva: WHO.
Neuberger, James. 2012. Rationing life-saving resources—how should allocation policies be assessed in solid organ transplantation: Criteria for organ allocation. Transplant International 25: 3–6. https://doi.org/10.1111/j.1432-2277.2011.01327.x.
NHS Choices. 2015. The Principles and Values of the NHS in England. May 28.
NHS Choices. 2016. Who Should Have the Flu Vaccine? July 12.
Office for National Statistics. 2016. National Life Tables, UK: 2013–2015. Office for National Statistics.
Osterweil, Neil. World Class Emergency Response in Boston Marathon Bombing. Medscape. October 28, 2015
Palazzo, Chiara, and Emily Allen. Manchester Terror Attack: Everything We Know. The Telegraph, May 24, 2017.
Persad, Govind, Alan Wertheimer, and Ezekiel J. Emanuel. 2009. Principles for allocation of scarce medical interventions. The Lancet 373: 423–431.
Pesik, Nicki, Mark E. Keim, and Kenneth V. Iserson. 2001. Terrorism and the ethics of emergency medical care. Annals of Emergency Medicine 37: 642–646. https://doi.org/10.1067/mem.2001.114316.
Rawlins, Michael D., and Anthony J. Culyer. 2004. National Institute for Clinical Excellence and its value judgments. BMJ: British Medical Journal 329: 224–227.
Rescher, Nicholas. 1969. The allocation of exotic medical lifesaving therapy. Ethics 79: 173–186.
Rivlin, M. M. 1995. Protecting elderly people: Flaws in ageist arguments. BMJ: British Medical Journal 310: 1179–1182.
Rivlin, Michael M. 2000. Why the fair innings argument is not persuasive. BMC Medical Ethics 1: 1. https://doi.org/10.1186/1472-6939-1-1.
Royal College of Peadiatrics and Child Health. 2017. Politicians Must Value Our Children as Much as the Elderly or Britain Faces “Serious Consequences”, Says Top Children’s Doctor. http://www.rcpch.ac.uk/news/politicians-must-value-our-children-much-elderly-or-britain-faces-serious-consequences-says-top. Accessed January 23.
Sanders, David, and Jesse Dukeminier Jr. 1967. Medical advance and legal lag: Hemodialysis and kidney transplantation. UCLA Law Revision 15: 357.
Savulescu, Julian, and Peter Singer. Unpicking What We Mean by Best Interests in Light of Charlie Gard. The BMJ Opinion. August 2, 2017.
Silva, Diego S., Jennifer L. Gibson, Ann Robertson, Cécile M. Bensimon, Sachin Sahni, Laena Maunula, and Maxwell J. Smith 2012. Priority setting of ICU resources in an influenza pandemic: A qualitative study of the Canadian public’s perspectives. BMC Public Health 12: 1.
Sprung, Charles L., Marion Danis, Gaetano Iapichino, Antonio Artigas, Jozef Kesecioglu, Rui Moreno, Anne Lippert et al. 2013. Triage of intensive care patients: Identifying agreement and controversy. Intensive Care Medicine 39: 1916–1924. https://doi.org/10.1007/s00134-013-3033-6.
Stewart, Rory. Our Culture Excludes the Old When They Have So Much to Contribute. The Guardian, sec. Opinion, November 9, 2013.
Teutsch, Steven, and Bernd Rechel. 2012. Ethics of resource allocation and rationing medical care in a time of fiscal restraint-US and Europe. Public Health Reviews 34: 15.
The Economist. Britain’s Efficiency Trap. The Economist, September 4, 2014.
Ventilator Document Workgroup. 2011. Ethical Considerations for Decision Making Regarding Allocation of Mechanical Ventilators During a Severe Influenza Pandemic or Other Public Health Emergency. Atlanta: Centers for Disease Control and Prevention.
Weale, Sally. Privately Educated Elite Continues to Take Top UK Jobs, Finds Survey. The Guardian, sec. Education, February 24, 2016.
White, Douglas B., Mitchell H. Katz, John M. Luce, and Bernard Lo. 2009. Who should receive life support during a public health emergency? Using ethical principles to improve allocation decisions. Annals of Internal Medicine 150: 132–138.
Acknowledgements
I would want to acknowledge Carol Buydos and Nathan Gamble for proof reading and comments, as well as Matt James and Trevor Stammers for comments and encouragement when a previous version of this work was submitted as a university assignment at St. Mary’s University Twickenham, London. I would also want to thank the two anonymous reviewers for their comments and suggestions. All mistakes in the text should be attributed the author. The views expressed in this text are the author’s and might not correspond with the views of any organization with which the author is associated or with the views of any people acknowledged here.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that he has no conflict of interest.
Rights and permissions
About this article
Cite this article
Pruski, M. Experience adjusted life years and critical medical allocations within the British context: which patient should live?. Med Health Care and Philos 21, 561–568 (2018). https://doi.org/10.1007/s11019-018-9830-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11019-018-9830-5