- 1Clinical Neuropsychology and Cognitive Neuroscience Centre, Music Cognition Laboratory, Department of Clinical Psychology, National Institute of Mental Health and Neuroscienes (NIMHANS), Bengaluru, India
- 2Clinical Neuropsychology and Cognitive Neuroscience Centre, Department of Clinical Psychology, Music Cognition Laboratory, Wellcome Trust/DBT India Alliance CPH - Intermediate Fellow (IA/CPHI/17/1/503348), National Institute of Mental Health and Neuroscienes (NIMHANS), Bengaluru, India
- 3Department of Biostatistics, NIMHANS, Bengaluru, India
- 4Department of Psychiatry, NIMHANS, Bengaluru, India
Background: Cognitive deficits are one of the core features of major depressive disorder (MDD) that play crucial role in functional recovery. Studies have explored cognitive deficits in MDD, however, given inconsistent results, especially in mild-moderate MDD. Recently, studies have explored music as cognitive ability in various clinical conditions. In MDD, large focus has been on evaluating emotion deficits and just a handful on music cognition. With growing evidence on use of music based intervention to target cognitive deficits, it is imperative to explore nature of music cognitive ability in MDD.
Aim: To examine musical and neuro-cognitive deficits in patients with mild-moderate MDD.
Methods: Patients diagnosed with mild or moderate MDD (n = 19) and matched healthy controls (HC) (n = 18) were evaluated on selected tests from NIMHANS Neuropsychological test battery and Montreal battery for evaluation of amusia (MBEA).
Results: MDD group performed significantly lower than HC on working memory (p = 0.007), verbal learning (p = 0.02) and retention (p = 0.03). Three indices were computed for a comprehensive evaluation. Groups did not differ significantly in any of the indices- focused attention, executive function, learning and memory as well as on music cognition. Focused attention and memory index predicted music cognition in HC and the combined group (MDD + HC) (p < 0.01). Attention alone contributed to 62.1% of variance in music cognition. Similarly, music cognition significantly predicted focused attention (p < 0.01).
Conclusion: Individuals with mild-moderate MDD show significant deficits in working memory, verbal learning and memory, however, not in music cognition. There exists a significant relationship between music cognition and attention, which could be implicated in use of music interventions to ameliorate cognitive deficits. Limitations of study include small sample size and heterogeneity. Future studies on larger cohort examining musical emotion perception and neurocognition is imperative to have deeper understanding of this debilitating condition.
Introduction
Cognitive dysfunction is one of the core features of major depressive disorder (MDD) and several studies have been carried out exploring the nature of neuro-cognitive deficits in MDD. Reviews and meta-analytic studies have reported significant deficits in cognitive domains such as attention, executive functions, verbal and visual retention of information in MDD (McDermott and Ebmeier, 2009; Rock et al., 2014; Kaser et al., 2017). Neuro-cognitive deficits impact functional recovery and quality of life in patients with depression (Jaeger et al., 2006; Conradi et al., 2011; Roca et al., 2015). These deficits are observed even in first episode depression and can persist during remission (Airaksinen et al., 2004; Biringer et al., 2007; Gonda et al., 2015). Interestingly, studies that have examined varying levels of depression severity have revealed contradictory findings owing to methodological differences (Landrø et al., 2001; Murphy et al., 2003; Shenal et al., 2003; Gorlyn et al., 2006; Russo et al., 2015). Some studies report that patients with mild depression perform equal to the controls on cognitive tests (Airaksinen et al., 2004). In comparison to other neuropsychiatric conditions such as schizophrenia, there are limited studies examining neurocognitive profile in patients with mild to moderate MDD and there seems to be no commonly agreed neurocognitive profile characterizing depression (Gorlyn et al., 2006).
In addition to neurocognitive functions, over the last one and a half decade, studies have examined emotion perception deficits in depression (Bouhuys et al., 1995; Kan et al., 2004; Péron et al., 2011; Van Vleet et al., 2019). In recent times, studies have been initiated to also examine music cognitive deficits and music emotion perception deficits in depression. The reasons for this are twofold. One, music cognitive deficits are being studied in par with other neurocognitive functions that have been traditionally evaluated. Two, music is a strong elicitor of emotion. Hence deficits in emotion perception and use of music-based intervention to help alleviate mood symptoms are being explored quite rigorously in the recent past (Naranjo et al., 2011; Aalbers et al., 2017). Yet, very little is known about music cognitive deficits in depression such as deficits in perception of musical features such as melodic contour, scale, rhythm perception and rhythmic contour.
Music cognition and major depression
Music has always been an integral part of human society (Fitch, 2006) and in the recent past, investigation of music perception and processing has been used as a key to understand human brain. Music perception, like language processing, involves hierarchically organized network and activation of cortical and subcortical brain areas that govern auditory perception, semantic processing, attention, memory and emotion (Koelsch, 2010; Sarkamo et al., 2013). Processing of music is thus considered emotionally laden, neuro-cognitive process. In depression, so far studies have mainly focused on understanding deficits in musical emotion and not so much on music cognition (Gotlib et al., 2004; Punkanen et al., 2011).
Music cognition is currently a growing research area bringing an information processing approach, combining music theory with cognitive neuro-science in understanding music perception. Only in the recent times, studies have explored music cognitive deficits in depression similar to other neurological and neuropsychiatric conditions such as stroke, Parkinson’s disease, schizophrenia (Schuppert et al., 2000; Särkämö et al., 2009, 2010; Hatada et al., 2014; Wen et al., 2014; Biswas et al., 2016; Fujito et al., 2018). Deficits in musical expression such as disrupted tempo while playing instrument, deficits in identifying and discrimination of music elements such as pitch, rhythm and melody have been reported in patients with depression (Steinberg and Raith, 1985; Schwenzer et al., 2012). A longitudinal follow up study reported impairment in melody comparison, rhythm perception and emotional categorization of music, which improved with symptom reduction during follow up in patients with severe depression (Reker et al., 2014). Musical deficits may be implicated in depression in several ways. Studies have linked musical deficits to deficits in vocal emotion perception (Nussbaum and Schweinberger, 2021). Individuals with MDD are reported to have difficulties in processing emotions presented via facial, vocal and musical stimuli (Naranjo et al., 2011). These deficits can interfere with social functioning and their interpersonal relationships. In addition, music processing such as rhythm perception and entrainment are seen as very basic perceptual processes occurring even before conscious cognitive mechanisms. Ability to perceive beat and rhythm is said to optimize attentional resources and has its links to core cognitive mechanisms such as attention and information processing (Jones, 1976; Large and Jones, 1999; Bolger et al., 2013; Smith et al., 2014; Bharathi et al., 2019). It is also important to note that, music perception deficits can be disabling even in individuals who are not professional musicians. In other words, musical deficits are known to have significant implications in the non-musical domains of cognitive functioning and has an impact on the individuals’ overall functioning including emotional and social functioning.
Given these common theoretical links and neural substrates between music and cognition, it opens up clear possibility of dense association between them. It is also interesting to note that musical activities are proven to be efficacious in improving cognitive functions in various psychiatric and neurological conditions (Maratos et al., 2008; Bradt et al., 2010; Thaut, 2010; Hegde, 2014; Leubner and Hinterberger, 2017; Massaia et al., 2018). However, studies exploring the relationship between music and neuro-cognition systematically are scarce. Deeper understanding about this association would further provide evidence and expand possibilities of development of music-based interventions targeting neurocognitive deficits in patients with depression.
Given this background and lack of any systematic study from the Indian subcontinent, the current study was carried out with the aim of exploring music-cognitive and neuro-cognitive deficits in patients with mild-moderate MDD.
Materials and methods
Participants
Patients aged between 18 and 45 years with formal education of 07 years, diagnosed with mild or moderate MDD as per the 10th revision of International Classification of diseases (ICD-10) (n = 19) and age, sex and education matched healthy controls (HC) (n = 18) comprised the sample. Patients were recruited from the outpatient services of a tertiary mental health and neuroscience institute, the National Institute of Mental Health and Neuro Sciences. Clinical evaluation of all the patients and confirmation of the diagnosis was carried out by a qualified psychiatrist (MK). Patients diagnosed with depressive episode as part of bipolar disorder, and those with suicidal attempts or tendencies were excluded from the study. Age, education and sex matched HC were recruited from the community. Individuals with any past history of other neurological/psychiatric illness or medical comorbidities were excluded from the study. All the participants were right-handed as screened on Edinburgh Handedness Inventory (Oldfield, 1971) and had no formal training in music or any other performing art forms for more than 2-years.
Procedure
The study protocol was approved by the Institute’s Ethics Committee. Written informed consent was obtained from all participants. The socio demographic and clinical details of the patient group were recorded. MDD and HC group were assessed on the below mentioned tools over 1–2 sessions, with adequate rest period in between. The assessments were carried out in a span of two session on a few patients who reported fatigue. Patients were debriefed about the findings and feedback was given after the assessment were completed.
Tools/scales
A socio-demographic sheet, a clinical data sheet and music behavior data sheets were prepared by the researcher which included basic demographic details, clinical details and musical preferences of the participants. A music behavior data sheet was prepared to collect information on participants’ musical preferences, details related to training, hours of listening, genre of preference and their perception and attitudes toward using music as a treatment modality. Participants were also asked to list subjectively perceived cognitive deficits and rate them on scale of 1–10, greater score corresponding to higher deficits.
The Hamilton Depression Rating Scale (HAMD) (Hamilton, 1986) was used to assess symptom severity of depression in patients.
Montreal Battery for Evaluation of Amusia (MBEA) was used to measure the music cognitive abilities. The MBEA allows the diagnosis amusia by assessing musical abilities related to six components of musical processing presented in the neuropsychological model of musical cognitive processing, namely: Contour, Scale, Interval, Rhythm, Meter, and Musical Memory (Peretz et al., 2003).
Selected tests from NIMHANS Neuropsychological test battery and Wechsler’s Memory Scale (Pushpalatha, 2004; Rao et al., 2004) were used to evaluate the neurocognitive functions. The tests used to assess the neurocognitive functions were as follows—Color trails test (D’Elia et al., 1996) to assess focused attention and cognitive flexibility (Color trails-2), Verbal N back test (Smith and Jonides, 1999) to assess verbal working memory, Spatial Span test, WMS-III India (Pushpalatha, 2004) to assess visual working memory, Stroop color-word test (Golden and Freshwater, 2002) to assess response inhibition, Rey’s Auditory Verbal Learning test (RAVLT) (Maj et al., 1994) to assess verbal learning and memory, and Rey’s Osterrieth Complex Figure Test (CFT) (Rey, 1941) to assess visual construction and memory.
Statistical analysis
Data was coded for analysis using SPSS version 22.0 for Windows. Descriptive statistics such as mean, standard deviation and percentages were used to describe the socio-demographic data. Normality of data was assessed using Shapiro Wilks Test and Kolmogorov Smirnov Test.
Computation of neurocognitive indices
Six tests were used to measure various domains of neurocognitive functions. In order to compare the groups on neurocognitive domains—focused attention, executive functions and memory, three composite neurocognitive indices were obtained. The raw scores of each of the test were rescaled using min-max normalization to make the scores of different tests comparable. Mix-max normalization is a normalization strategy that scales the data between 0 and 1. It was calculated by subtracting the raw score from minimum value of the data set and then dividing it by the range (maximum value-minimum value). Composite executive function score was obtained by averaging the normalized scores of color trails 2, spatial span test, verbal N-Back 2 (hit score) and Stroop test. Composite learning and memory score were obtained by averaging normalized scores of AVLT (AVLT total, AVLT immediate recall and AVLT delayed recall) and CFT (CFT copy, CFT immediate recall and CFT delayed recall scores). Normalized score of Color trails 1 was considered as the focused attention score.
The performance of MDD and HC groups were compared on individual neurocognitive domains, neurocognitive indices and music cognition. Independent sample t-test was used to compare the groups for variables that assumed normality and Mann-Whitney U-test was applied to variables that violated the assumptions of normality. Welch Correction was applied wherever homogeneity of variance was not met. Appropriate correlation tests were used to understand the relationship between neurocognitive variables and music cognition. A stepwise linear regression was attempted in order to study the relationship between neurocognitive indices and music cognition.
Results
Socio-demographic and clinical status of the participants
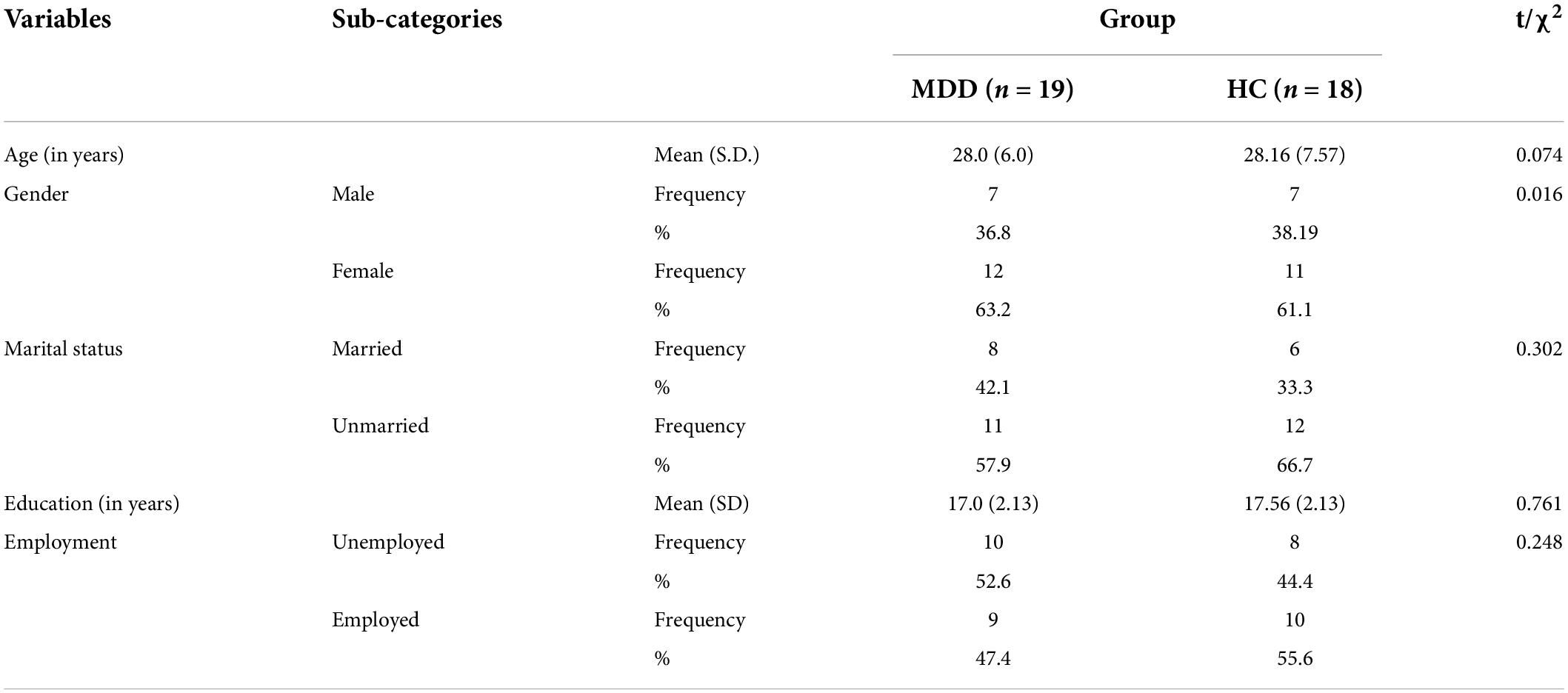
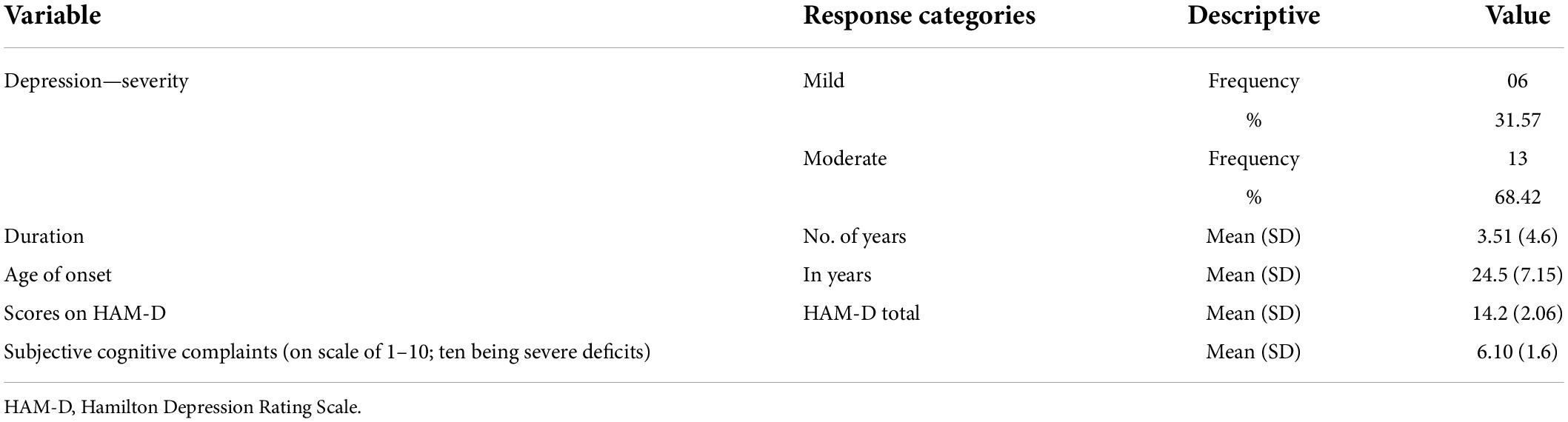
Sample comprised of 19 patients diagnosed with MDD [MDD: n = 19; M: F = 7:12; Mean age (years) 28 ± 6] and age, sex and education matched healthy participants [HC: n = 18; M: F = 7:11 Mean age (years) 28.1 ± 7.5]. The two groups did not differ significantly on any of the socio-demographic variables (Table 1). Table 2 shows clinical status of MDD group. Patient sample consisted of 6 (31.57%) patients with mild depression and 13 patients (68.42%) with moderate depression. The mean age of onset was 24.50 ± 7.15 years with a range of 13–43 years. Eleven patients (57.9%) were receiving individual psychotherapy. The mean HAM-D score was 14.3 ± 2.06, with range of 10–17. The mean score of subjectively reported cognitive deficits was found to be 6.10 ± 1.60. Patients reported difficulties mostly in domain of concentration and memory (especially remembering conversations, instructions).
Musical background and preferences of participants
As noted using the music behavior data sheet, a large percentage of both MDD (94.8%) and HC (100%) reported that they enjoyed listening to music. There was no significant difference between the two groups in terms of hours spent listening to music. Most participants (52.6% MDD vs. 50% HC) listened to music for more than 3 h in a week. Forty two percent of MDD patients and 33% of HC group had family members who were trained in music. Majority of the MDD and HC participants preferred concentrating on both lyrics and tune while listening to music (84% MDD vs. 89% HC). Also, majority of the participants opined that music can be used in treatment of psychiatric disorders. Participants self-reported a subjective evaluation of their ability to follow a rhythm, and keep a tune on a scale of 1–5, greater score corresponding to greater ability. There were no significant differences between MDD and HC on self-reported ability to remember tunes (3.5 HC vs. 3.8 MDD) as well as to keep rhythm (3.9 HC vs. 2.9 MDD).
Neurocognitive profile of major depressive disorder and healthy controls group
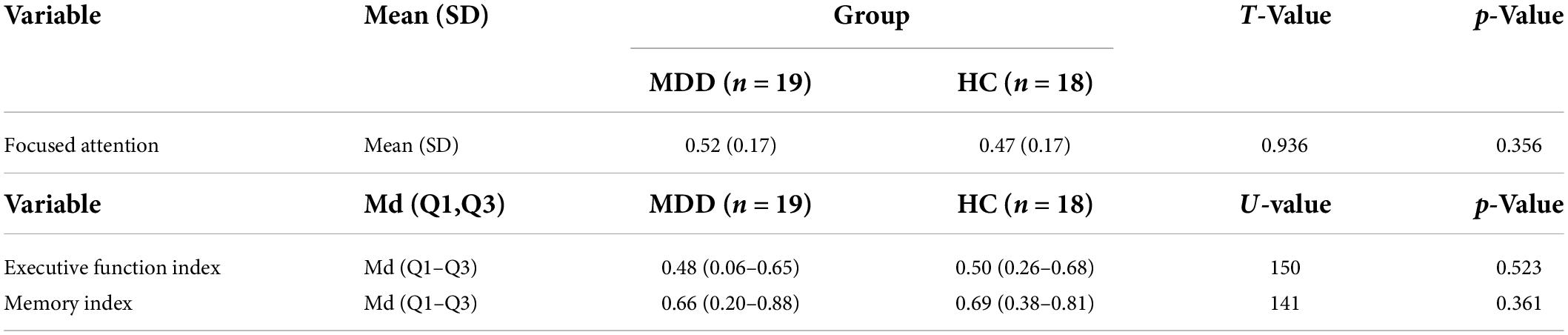
Tables 3, 4 shows the comparative performance of MDD and HC on tests of neurocognitive functioning. MDD group did not significantly differ from HC group on focused attention, executive function and learning and memory indices in general though MDD group obtained lower index scores as compared to HC. However, when individual test performance was compared between MDD and HC group, it was found that, the MDD group performed significantly lower on tasks assessing working memory (p = 0.007; < 0.01 level), verbal learning (p = 0.02; at 0.05 level) and delayed recall (AVLT) (p = 0.035; 0.05 level).
Music cognition among major depressive disorder and healthy controls group
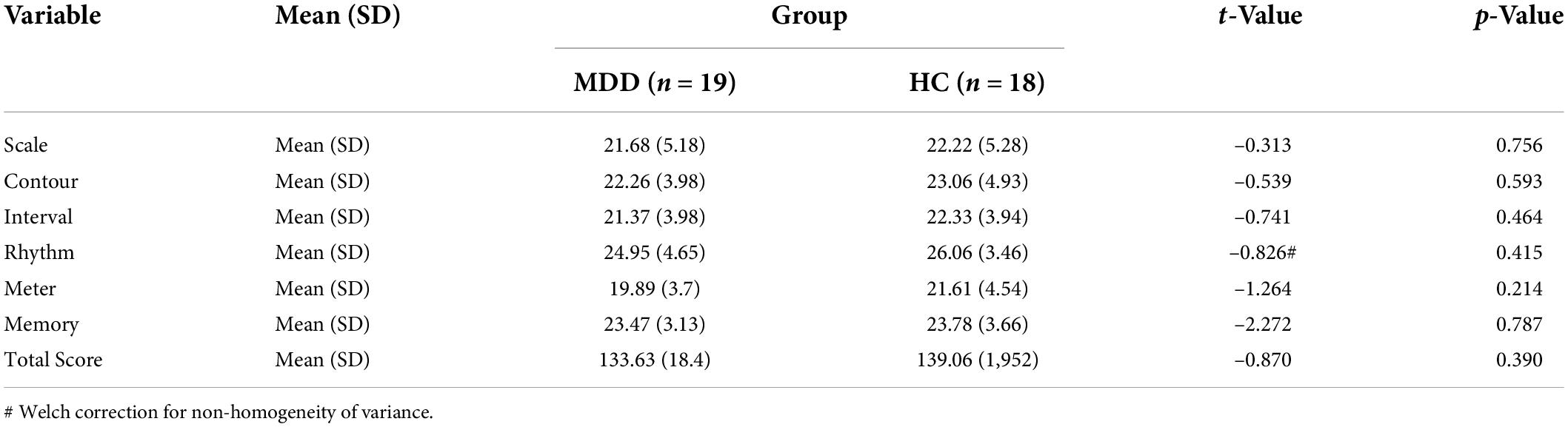
Table 5 shows the comparative performance of MDD and HC on test of music cognition. The groups did not significantly differ in their abilities to perceive musical differences on any of the music cognition domains– scale, contour, interval, rhythm, meter and memory. However, on mean comparison it is found that, the MDD group had underperformed (had lower scores) on all domains of music cognition.
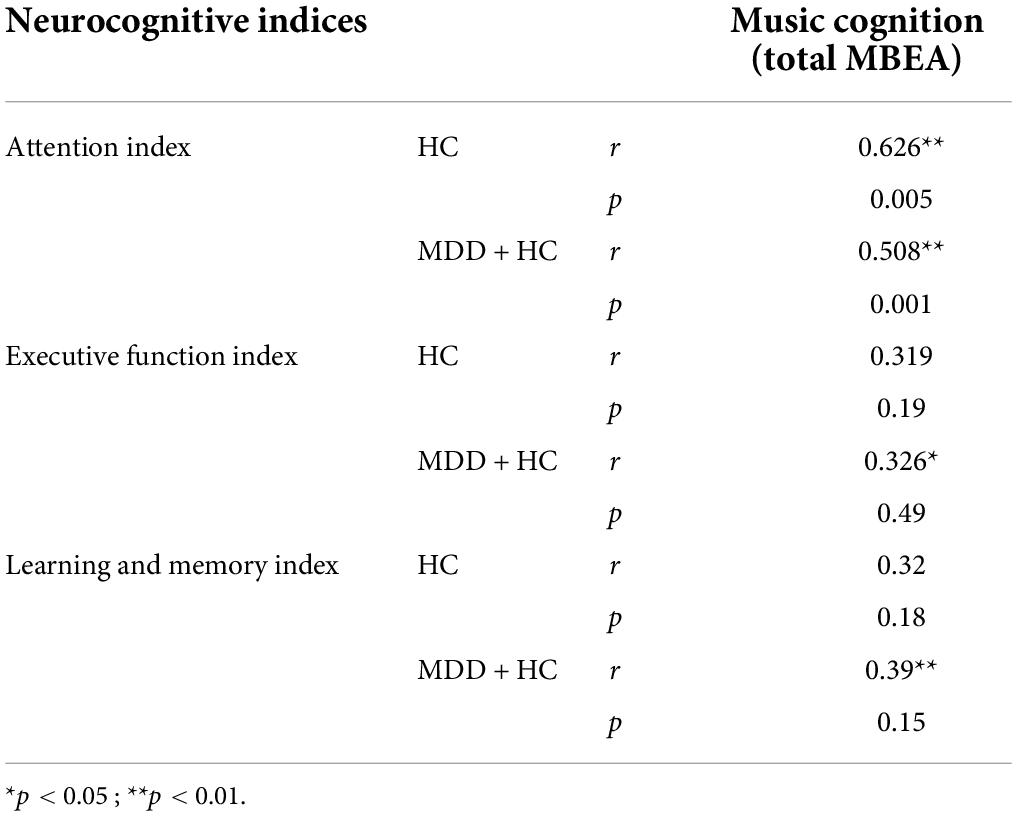
Relationship between neuro-cognition and music cognition
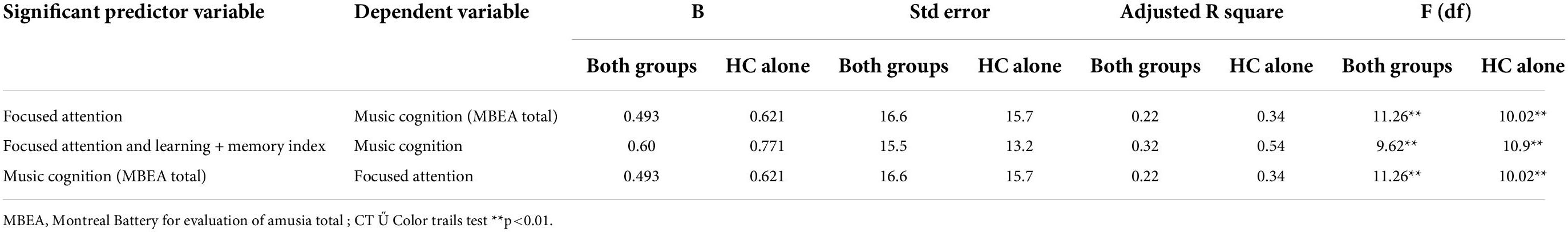
Stepwise linear regression was carried out to explore relationship between music-cognition and neurocognition in combined (MDD + HC) groups and healthy control alone group (HC) (Table 6). Dependent variable to be entered in regression analysis was identified based on significant findings on the correlation analysis (Table 7). Focused attention and memory index were found to be significant predictors of music cognition in HC and the combined group (MDD + HC) (p < 0.01). Attention and memory indices together were seen to predict 60.1 and 77.1% of music cognition variance in combined group and HC group, respectively. Attention alone contributed to 62.1% of variance in music cognition among HC group. In addition, music cognition significantly predicted focused attention (p < 0.01) (Table 6).
Discussion
The present study investigated music cognition and neuro-cognition in MDD compared to age, education and sex matched HC. It was observed that MDD underperformed on all the neurocognitive indices. The findings revealed significant differences between the groups on working memory, verbal encoding and retention. These findings are partly consistent with research findings reported in the field that have demonstrated presence of neurocognitive deficits in domains of executive functions (Harvey et al., 2005), attention and concentration (Kampf-Sherf et al., 2004), verbal and visual memory (Fossati et al., 1999; Zubieta et al., 2001). The findings from the present study did not show global cognitive deficits as documented in some of the previous studies. The circumscribed cognitive deficits could be explained by inconsistencies in association between depression and neuro-cognition in general (Austin et al., 2001; Wang et al., 2006; Gualtieri and Morgan, 2008). Most studies that have explored neurocognitive functioning in depression have not controlled for the severity of depression, which is known to have positive association with cognitive deficits (McDermott and Ebmeier, 2009). Patients with mild depression show lesser degree of deficits in executive function (Elderkin-Thompson et al., 2004).
Findings from the present study showed no significant differences between HC and MDD in the domain of music cognition. Very few studies are available that have explored music as cognitive variable and they have established music cognition deficits and evidences of abnormalities in auditory processing in certain conditions including depression (Steinberg and Raith, 1985; Michael et al., 2004; Tollkötter et al., 2006; Chase et al., 2010; Reker et al., 2014; Kraus et al., 2019). Music perception ability has been closely linked with neurocognitive functions such as attention, executive functions and visuo-spatial abilities (Särkämö et al., 2009; Wen et al., 2014). The pitch, rhythm, contour and interval discrimination subtests along with memory subtest, places high demand on cognitive functions including attention and working memory. In the current study, the MDD group did not have global cognitive impairment and seems to have relatively preserved cognitive abilities. This could one of the possible reasons for preserved musical abilities.
In this study we also observed a close link between focused attention with music cognition interestingly in combined group (MDD + HC) and HC alone, but not in MDD group. This could be explained by neurocognitive deficits in MDD group. Though, MDD and HC did not significantly differ on indices, individual domain analysis revealed deficits specifically in working memory, learning and memory.
In the current study, of all neurocognitive indices, focused attention was found to significantly predict music cognition. In addition, music cognition significantly predicted focused attention. Studies have shown bi-directional relationship between cognitive functions and music perception. Components of music such as timing, grouping and organization facilitates attentional processes by interacting with attention oscillators (Thaut, 2010; Thaut and Hoemberg, 2014). As mentioned earlier, ability to perceive rhythm could act as precursor to conscious cognitive processes including information processing, attention and memory. On other hand, It is also established that focusing and keeping track of music in time activates attentional and working memory network bilaterally, however, with activity in right hemisphere being more dominant (Sihvonen et al., 2017). Engaging in musical activities ranging from simple pitch and rhythm discriminating tasks to complex activities such as singing, listening, playing instrument, music production and improvisation can involve higher order cognitive processes.
In recent past, music-based interventions have been proven to be efficacious in improving neuro-cognitive functions including attention, executive functions and memory in several clinical conditions (Knott, 2017; Tumuluri et al., 2017; He et al., 2018; Jones et al., 2021). Cognitive remediation in depression in gaining its due importance in the field and music based interventions can prove to be beneficial. Although few in number, a few studies have shown positive results in depression as well in targeting cognition and emotional disturbances (Chu et al., 2014; Tai et al., 2015). Probably, a relatively well-preserved music cognitive ability can act as a mediating factor in effectiveness of music-based interventions in depression.
Conclusion
In conclusion, patients with mild-moderate depression perform poorly than HC in neurocognitive domains such as working memory, verbal encoding and retention, however, do not significantly differ from HC in music cognitive ability. Neuro-cognition and music cognition are found to significantly relate to each other.
Current study can be considered as an exploratory study. The present study has certain limitations. The sample size was small leading to limited generalizability of the findings. The sample was heterogeneous in terms of certain clinical variables such as age of onset, duration of illness and medications/therapy. There was a preponderance of females over males in the study.
Most studies available have explored music emotion perception and processing. And, there is clear dearth of studies aiming at understanding music cognition deficits in relation to neuro-cognition in affective disorders. Further, studies can also explore music emotion processing and its links with music cognition and neuro-cognition in affective disorders. Most patients in the present study enjoyed listening to music and 90% of them endorsed the view that music could be a tool for psychological interventions in the disorder which also strengthens the need to explore further and integrate music-based interventions to routine treatment options, especially those rooted in neuroscientific evidence.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Institute Ethics Committee, National Institute of Mental Health and Neurosciences. The patients/participants provided their written informed consent to participate in this study.
Author contributions
PAR worked on the research protocol, reviewed the literature, collected the data, carried out the data analysis and wrote the manuscript. SH conceptualized the study, designed the method, edited, and finalized the manuscript. MP contributed to study design, data analysis, and interpretation. MK contributed to the study design, clinical evaluation of patients recruited in the study, and contributed in finalizing the manuscript. The final article has been approved by all the authors of the current study.
Acknowledgments
We thank Dr. Prathyusha, Research Assistant, Department of Biostatistics, NIMHANS, Bengaluru for assisting with data entry and analysis. We thank all the participants for consenting to participate in this study. SH is a Clinical and Public Health- 2018 Intermediate Fellow of the Wellcome Trust-DBT India Alliance (IA/CPHI/17/1/503348).
Funding
This study was supported by the University Grants Commission (UGC), Ministry of Human Resource and Development, Government of India through the grant number 367/(NET-JULY2016).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Aalbers, S., Fusar-Poli, L., Freeman, R. E., Spreen, M., Ket, J. C., and Vink, A. C. (2017). Music therapy for depression. Cochrane Database Syst. Rev. 11:CD004517. doi: 10.1002/14651858.CD004517.pub3
Airaksinen, E., Larsson, M., Lundberg, I., and Forsell, Y. (2004). Cognitive functions in depressive disorders: evidence from a population-based study. Psychol. Med. 34, 83–91. doi: 10.1017/S0033291703008559
Austin, M.-P., Mitchell, P., and Goodwin, G. M. (2001). Cognitive deficits in depression: possible implications for functional neuropathology. Brit. J. Psychiatry 178, 200–206. doi: 10.1192/bjp.178.3.200
Bharathi, G., Kaavya, J., Balasubramanian, V., and Balachandar, V. (2019). The potential role of rhythmic entrainment and music therapy intervention for individuals with autism spectrum disorders. J. Exerc. Rehabil. 15, 180–186. doi: 10.12965/jer.1836578.289
Biringer, E., Mykletun, A., Sundet, K., Kroken, R., Stordal, K. I., and Lund, A. (2007). A longitudinal analysis of neurocognitive function in unipolar depression. J. Clin. Exp. Neuropsychol. 29, 879–891. doi: 10.1080/13803390601147686
Biswas, A., Hegde, S., Jhunjhunwala, K., and Pal, P. K. (2016). Two sides of the same coin: impairment in perception of temporal components of rhythm and cognitive functions in Parkinson’s disease. Basal Ganglia 6, 63–70. doi: 10.1016/j.baga.2015.12.001
Bolger, D., Trost, W., and Schön, D. (2013). Rhythm implicitly affects temporal orienting of attention across modalities. Acta Psychol. 142, 238–244. doi: 10.1016/j.actpsy.2012.11.012
Bouhuys, A. L., Bloem, G. M., and Groothuis, T. G. (1995). Induction of depressed and elated mood by music influences the perception of facial emotional expressions in healthy subjects. J. Affect. Disord. 33, 215–226. doi: 10.1016/0165-0327(94)00092-N
Bradt, J., Magee, W. L., Dileo, C., Wheeler, B. L., and McGilloway, E. (2010). Music therapy for acquired brain injury. Cochrane Database Syst. Rev. 7:Cd006787. doi: 10.1002/14651858.CD006787.pub2
Chase, H. W., Michael, A., Bullmore, E. T., Sahakian, B. J., and Robbins, T. W. (2010). Paradoxical enhancement of choice reaction time performance in patients with major depression. J. Psychopharmacol. 24, 471–479. doi: 10.1177/0269881109104883
Chu, H., Yang, C. Y., Lin, Y., Ou, K. L., Lee, T. Y., O’Brien, A. P., et al. (2014). The impact of group music therapy on depression and cognition in elderly persons with dementia: a randomized controlled study. Biol. Res. Nurs. 16, 209–217. doi: 10.1177/1099800413485410
Conradi, H., Ormel, J., and De Jonge, P. (2011). Presence of individual (residual) symptoms during depressive episodes and periods of remission: a 3-year prospective study. Psychol. Med. 41:1165. doi: 10.1017/S0033291710001911
Elderkin-Thompson, V., Boone, K. B., Hwang, S., and Kumar, A. (2004). Neurocognitive profiles in elderly patients with frontotemporal degeneration or major depressive disorder. J. Int. Neuropsychol. Soc. 10, 753–771. doi: 10.1017/S1355617704105067
Fitch, W. T. (2006). The biology and evolution of music: a comparative perspective. Cognition 100, 173–215. doi: 10.1016/j.cognition.2005.11.009
Fossati, P., Amar, G., Raoux, N., Ergis, A. M., and Allilaire, J. F. (1999). Executive functioning and verbal memory in young patients with unipolar depression and schizophrenia. Psychiatry Res. 89, 171–187. doi: 10.1016/S0165-1781(99)00110-9
Fujito, R., Minese, M., Hatada, S., Kamimura, N., Morinobu, S., Lang, D. J., et al. (2018). Musical deficits and cortical thickness in people with schizophrenia. Schizophr. Res. 197, 233–239. doi: 10.1016/j.schres.2018.01.027
Golden, C. J., and Freshwater, S. M. (2002). Stroop Color and Word Test Kit for Adults. Delhi: Psycho Matrix. doi: 10.1037/t06065-000
Gonda, X., Pompili, M., Serafini, G., Carvalho, A. F., Rihmer, Z., and Dome, P. (2015). The role of cognitive dysfunction in the symptoms and remission from depression. Ann. Gen. Psychiatr. 14:27. doi: 10.1186/s12991-015-0068-9
Gorlyn, M., Keilp, J. G., Oquendo, M. A., Burke, A. K., Sackeim, H. A., and John Mann, J. (2006). The WAIS-III and major depression: absence of VIQ/PIQ differences. J. Clin. Exp. Neuropsychol. 28, 1145–1157. doi: 10.1080/13803390500246944
Gotlib, I. H., Krasnoperova, E., Neubauer, D., and Joormann, J. (2004). Attentional biases for negative interpersonal stimuli in clinical depression. J. Abnormal Psychol. 113, 127–135. doi: 10.1037/0021-843X.113.1.121
Gualtieri, C. T., and Morgan, D. W. (2008). The frequency of cognitive impairment in patients with anxiety, depression, and bipolar disorder: an unaccounted source of variance in clinical trials. J. Clin. Psychiatry 69, 1122–1130. doi: 10.4088/JCP.v69n0712
Hamilton, M. (1986). “The Hamilton Rating Scale for Depression,” in Assessment of Depression, eds N. Sartorius and T. A. Ban (Berlin, Heidelberg: Springer). doi: 10.1007/978-3-642-70486-4_14
Harvey, P.-O., Fossati, P., Pochon, J.-B., Levy, R., LeBastard, G., and Lehéricy, S. (2005). Cognitive control and brain resources in major depression: an fMRI study using the n-back task. Neuroimage 26, 860–869. doi: 10.1016/j.neuroimage.2005.02.048
Hatada, S., Sawada, K., Akamatsu, M., Doi, E., Minese, M., and Yamashita, M. (2014). Impaired musical ability in people with schizophrenia. J. Psychiatry Neurosci. 39, 118–126. doi: 10.1503/jpn.120207
He, H., Yang, M., Duan, M., Chen, X., Lai, Y., and Xia, Y. (2018). Music Intervention Leads to Increased Insular Connectivity and Improved Clinical Symptoms in Schizophrenia. Front. Neurosci. 11:744. doi: 10.3389/fnins.2017.00744
Hegde, S. (2014). Music-Based Cognitive Remediation Therapy for Patients with Traumatic Brain Injury. Front. Neurol. 5:34. doi: 10.3389/fneur.2014.00034
Jaeger, J., Berns, S., Uzelac, S., and Davis-Conway, S. (2006). Neurocognitive deficits and disability in major depressive disorder. Psychiatry Res. 145, 39–48. doi: 10.1016/j.psychres.2005.11.011
Jones, C., Richard, N., and Thaut, M. (2021). Investigating music-based cognitive rehabilitation for individuals with moderate to severe chronic acquired brain injury: a feasibility experiment. NeuroRehabilitation 48, 209–220. doi: 10.3233/NRE-208015
Jones, M. R. (1976). Time, our lost dimension: toward a new theory of perception, attention, and memory. Psychol. Rev. 83, 323–355. doi: 10.1037/0033-295X.83.5.323
Kampf-Sherf, O., Zlotogorski, Z., Gilboa, A., Speedie, L., Lereya, J., Rosca, P., et al. (2004). Neuropsychological functioning in major depression and responsiveness to selective serotonin reuptake inhibitors antidepressants. J. Affect. Disord. 82, 453–459. doi: 10.1016/j.jad.2004.02.006
Kan, Y., Mimura, M., Kamijima, K., and Kawamura, M. (2004). Recognition of emotion from moving facial and prosodic stimuli in depressed patients. J. Neurol. Neurosurg. Psychiatry 75, 1667–1671. doi: 10.1136/jnnp.2004.036079
Kaser, M., Zaman, R., and Sahakian, B. J. (2017). Cognition as a treatment target in depression. Psychol. Med. 47, 987–989. doi: 10.1017/S0033291716003123
Knott, D. (2017). Musical mnemonics training: proposed mechanisms and case example with acquired brain injury. Music Ther. Perspect. 35, 23–29. doi: 10.1093/mtp/miv016
Koelsch, S. (2010). Towards a neural basis of music-evoked emotions. Trends Cogn. Sci. 14, 131–137. doi: 10.1016/j.tics.2010.01.002
Kraus, M. S., Walker, T. M., Jarskog, L. F., Millet, R. A., and Keefe, R. S. E. (2019). Basic auditory processing deficits and their association with auditory emotion recognition in schizophrenia. Schizophr. Res. 204, 155–161. doi: 10.1016/j.schres.2018.08.031
Landrø, N. I., Stiles, T. C., and Sletvold, H. (2001). Neuropsychological function in nonpsychotic unipolar major depression. Neuropsychiatry Neuropsychol. Behav. Neurol. 14, 233–240.
Large, E. W., and Jones, M. R. (1999). The dynamics of attending: how people track time-varying events. Psychol. Rev. 106, 119–159. doi: 10.1037/0033-295X.106.1.119
Leubner, D., and Hinterberger, T. (2017). Reviewing the effectiveness of music interventions in treating depression. Front. Psychol. 8:1109. doi: 10.3389/fpsyg.2017.01109
Maj, M., Satz, P., Janssen, R., Zaudig, M., Startace, F., D’Elia, L. F., et al. (1994). WHO Neuropsychiatric AIDS study, cross sectional phase II: neuropsychological and neurological findings. Arch. Gen. Psychiatry 51, 51–61. doi: 10.1001/archpsyc.1994.03950010051007
Maratos, A., Gold, C., Wang, X., and Crawford, M. (2008). Music therapy for depression. Cochrane Database Syst. Rev. 2017:CD004517. doi: 10.1002/14651858.CD004517.pub2
Massaia, M., Reano, A., Luppi, C., Santagata, F., Marchetti, M., and Isaia, G. C. (2018). Receptive music interventions improve apathy and depression in elderly patients with dementia. Geriatr. Care 4, 8–15. doi: 10.4081/gc.2018.7248
McDermott, L. M., and Ebmeier, K. P. (2009). A meta-analysis of depression severity and cognitive function. J. Affect. Disord. 119, 1–8. doi: 10.1016/j.jad.2009.04.022
Michael, N., Ostermann, J., Sörös, P., Schwindt, W., and Pfleiderer, B. (2004). Altered Habituation in the Auditory Cortex in a Subgroup of Depressed Patients by Functional Magnetic Resonance Imaging. Neuropsychobiology 49, 5–9. doi: 10.1159/000075331
Murphy, F., Michael, A., Robbins, T., and Sahakian, B. (2003). Neuropsychological impairment in patients with major depressive disorder: the effects of feedback on task performance. Psychol. Med. 33, 455–467. doi: 10.1017/S0033291702007018
Naranjo, C., Kornreich, C., Campanella, S., Noel, X., Vandriette, Y., and Gillain, B. (2011). Major depression is associated with impaired processing of emotion in music as well as in facial and vocal stimuli. J. Affect. Disord. 128, 243–251. doi: 10.1016/j.jad.2010.06.039
Nussbaum, C., and Schweinberger, S. (2021). Links Between Musicality and Vocal Emotion Perception. Emot. Rev. 13, 211–224. doi: 10.1177/17540739211022803
Oldfield, R. C. (1971). The assessment and analysis of handedness: the Edinburgh Inventory. Neuropsychologia 9, 97–113. doi: 10.1016/0028-3932(71)90067-4
Peretz, I., Champod, A. S., and Hyde, K. (2003). Varieties of musical disorders: the Montreal Battery of Evaluation of Amusia. Ann. N. Y. Acad. Sci. 999, 58–75. doi: 10.1196/annals.1284.006
Péron, J., El Tamer, S., Grandjean, D., Leray, E., Travers, D., and Drapier, D. (2011). Major depressive disorder skews the recognition of emotional prosody. Prog. Neuropsychopharmacol. Biol. Psychiatry. 35, 987–996. doi: 10.1016/j.pnpbp.2011.01.019
Punkanen, M., Eerola, T., and Erkkila, J. (2011). Biased emotional recognition in depression: perception of emotions in music by depressed patients. J. Affect. Disord. 130, 118–126. doi: 10.1016/j.jad.2010.10.034
Pushpalatha, G. (2004). Adaptation and standardization of Wechsler memory scale. Ph.D. thesis. Bangalore: Department of Mental Health and Social Psychology, NIMHANS.
Rao, S. L., Subbakrishna, D. K., and Gopukumar, K. (2004). NIMHANS Neuropsycholoy Battery-2004. Bangalore: NIMHANS Publication; 2004.
Reker, P., Domschke, K., Zwanzger, P., and Evers, S. (2014). The impact of depression on musical ability. J. Affect. Disord. 156, 150–155. doi: 10.1016/j.jad.2013.12.010
Rey, A. (1941). Psychological Examination of Traumatic Encephalopathy. Archives de Psychologie 28, 286–340.
Roca, M., Monzón, S., Vives, M., López-Navarro, E., Garcia-Toro, M., and Vicens, C. (2015). Cognitive function after clinical remission in patients with melancholic and non-melancholic depression: a 6 month follow-up study. J. Affect. Disord. 171, 85–92. doi: 10.1016/j.jad.2014.09.018
Rock, P. L., Roiser, J. P., Riedel, W. J., and Blackwell, A. D. (2014). Cognitive impairment in depression: a systematic review and meta-analysis. Psychol. Med. 44, 2029–2040. doi: 10.1017/S0033291713002535
Russo, M., Mahon, K., and Burdick, K. E. (2015). Measuring cognitive function in MDD: emerging assessment tools. Depress. Anxiety 32, 262–269. doi: 10.1002/da.22297
Sarkamo, T., Tervaniemi, M., and Huotilainen, M. (2013). Music perception and cognition: development, neural basis, and rehabilitative use of music. Wiley Interdiscip. Rev. Cogn. Sci. 4, 441–451. doi: 10.1002/wcs.1237
Särkämö, T., Tervaniemi, M., Soinila, S., Autti, T., Silvennoinen, H. M., and Laine, M. (2009). Cognitive deficits associated with acquired amusia after stroke: a neuropsychological follow-up study. Neuropsychologia 47, 2642–2651. doi: 10.1016/j.neuropsychologia.2009.05.015
Särkämö, T., Tervaniemi, M., Soinila, S., Autti, T., Silvennoinen, H. M., and Laine, M. (2010). Auditory and Cognitive Deficits Associated with Acquired Amusia after Stroke: a Magnetoencephalography and Neuropsychological Follow-Up Study. PLoS One 5:e15157. doi: 10.1371/journal.pone.0015157
Schuppert, M., Münte, T. F., Wieringa, B. M., and Altenmüller, E. (2000). Receptive amusia: evidence for cross-hemispheric neural networks underlying music processing strategies. Brain 123, 546–559. doi: 10.1093/brain/123.3.546
Schwenzer, M., Zattarin, E., Grözinger, M., and Mathiak, K. (2012). Impaired pitch identification as a potential marker for depression. BMC Psychiatry 12:1–6. doi: 10.1186/1471-244X-12-32
Shenal, B. V., Harrison, D. W., and Demaree, H. A. (2003). The neuropsychology of depression: a literature review and preliminary model. Neuropsychol. Rev. 13, 33–42. doi: 10.1023/A:1022300622902
Sihvonen, A. J., Särkämö, T., Leo, V., Tervaniemi, M., Altenmüller, E., and Soinila, S. (2017). Music-based interventions in neurological rehabilitation. Lancet Neurol. 16, 648–660. doi: 10.1016/S1474-4422(17)30168-0
Smith, E. E., and Jonides, J. (1999). Storage and executive processes in the frontal lobes. Science 283, 1657–1661. doi: 10.1126/science.283.5408.1657
Smith, R., Rathcke, T., Cummins, F., Overy, K., and Scott, S. (2014). Communicative rhythms in brain and behaviour. Philos. Trans. R. Soc. Lond. B. Biol. Sci. 369:20130389. doi: 10.1098/rstb.2013.0389
Steinberg, R., and Raith, L. (1985). Music Psychopathology. Psychopathology 18, 254–264. doi: 10.1159/000284413
Tai, S.-Y., Wang, L.-C., and Yang, Y.-H. (2015). Effect of music intervention on the cognitive and depression status of senior apartment residents in Taiwan. Neuropsychiatr Dis .Treat. 11, 1449–1454. doi: 10.2147/NDT.S82572
Thaut, M. H. (2010). Neurologic Music Therapy in Cognitive Rehabilitation. Music Percept. Interdiscipl. J. 27:281. doi: 10.1525/mp.2010.27.4.281
Thaut, M., and Hoemberg, V. (2014). Handbook of neurologic music therapy. Oxford: Oxford University Press.
Tollkötter, M., Pfleiderer, B., Sörös, P., and Michael, N. (2006). Effects of antidepressive therapy on auditory processing in severely depressed patients: a combined MRS and MEG study. J. Psychiatr. Res. 40, 293–306. doi: 10.1016/j.jpsychires.2005.09.003
Tumuluri, I., Hegde, S., and Nagendra, H. R. (2017). Effectiveness of Music Therapy on Focused Attention, Working Memory and Stress in Type 2 Diabetes: an Exploratory Study. Int. J. Yoga 10, 167–170. doi: 10.4103/0973-6131.213471
Van Vleet, T., Stark, A., Merzenich, M. M., Jordan, J., Wallace, D. L., Lee, M. B., et al. (2019). Biases in Processing of Mood-Congruent Facial Expressions in Depression. Psychiatry Res. 275, 143–148. doi: 10.1016/j.psychres.2019.02.076
Wang, C. E., Halvorsen, M., Sundet, K., Steffensen, A. L., Holte, A., and Waterloo, K. (2006). Verbal memory performance of mildly to moderately depressed outpatient younger adults. J. Affect. disorders 92, 283–286. doi: 10.1016/j.jad.2006.02.008
Wen, Y., Nie, X., Wu, D., Liu, H., Zhang, P., and Lu, X. (2014). Amusia and cognitive deficits in schizophrenia: is there a relationship? Schizophr. Res. 157, 60–62. doi: 10.1016/j.schres.2014.05.029
Keywords: depression, neuro-cognition, music-cognition, attention, executive functions, memory
Citation: Raghavendra PA, Hegde S, Philip M and Kesavan M (2022) Music and neuro-cognitive deficits in depression. Front. Psychol. 13:959169. doi: 10.3389/fpsyg.2022.959169
Received: 01 June 2022; Accepted: 11 July 2022;
Published: 04 August 2022.
Edited by:
Fabrizio Stasolla, Giustino Fortunato University, ItalyReviewed by:
Giuseppina Spano, University of Bari Aldo Moro, ItalyKriti Mishra, Lincoln County Hospital, United Kingdom
Copyright © 2022 Raghavendra, Hegde, Philip and Kesavan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shantala Hegde, shantala.hegde@gmail.com, shegde@nimhans.ac.in
 Prathima A. Raghavendra
Prathima A. Raghavendra Shantala Hegde
Shantala Hegde Mariamma Philip3
Mariamma Philip3 Muralidharan Kesavan
Muralidharan Kesavan