Abstract
Current United States guidelines for neonatal resuscitation note that there is no mandate to resuscitate infants in all situations. For example, the fetus that at the time of delivery is determined to be so premature as to be non-viable need not be aggressively resuscitated. The hypothetical case of an extremely premature infant was presented to neonatologists from the United States and four other European countries at a September 2006 international meeting sponsored by the World Health Organization Collaborating Center in Reproductive Health of Atlanta (currently, the Global Collaborating Center in Reproductive Health). Responses to the case varied by country, due to differences in legal, ethical and related practice parameters, rather than differences in medical technology, as similar medical technology was available within each country. Variations in approach seemed to stem from physicians’ perceptions of their ability to remove the neonate from life support if this appeared non-beneficial. There appears to be a desire for greater convergence in practice options and more open discussion regarding the practical problems underlying the variability. Specifically, the conference attendees identified four areas that need to be addressed: (1) lack of international consensus guidelines in viability and therapeutic options, (2) lack of bodies capable of generating these guidelines, (3) variation in laws between countries, and (4) the frequent failure of physicians and families to confront death at the beginning of life.
Similar content being viewed by others
Introduction
The Global Collaborating Center in Reproductive Health (formerly, the World Health Organization Collaborating Center in Reproductive Health, or “the Center”) in Atlanta, GA, USA, states as its primary vision, “to improve every family’s chances for a healthy and wanted pregnancy and a healthy outcome for every mother and child—and that following child birth, the mother and infant are alive and healthy and the infant is safe and loved” (McCarthy B. and Brann A. Vision and Mission Statement, World Health Organization Collaborating Center in Reproductive Health [currently, the Global Collaborating Center in Reproductive Health], 1992, 2002, 2010). In order to address issues of international and intra-national collaborative system development, the Center recognized a number of years ago that the ethics of professionalism and patient care must be addressed in concert with modern clinical and system-based training in order to assure that quality care was not compromised for any reason. The issues of neonatal resuscitation and the specifics of resuscitation in the marginally viable neonate present challenges in every country. Therefore, this topic was chosen as the theme for the Center’s first International Ethics Symposium: Global Issues in Neonatal Resuscitation. This paper reviews the program and discussion of the participants at that conference. The comments in this paper reflect those made during program development and program execution by international participants, each of whom was actively doing intensive neonatal-perinatal care in his or her respective country.
Background and WHO/Russian Collaboration
The Center is a partnership between the Woodruff Health Sciences Center of Emory University, the National Centers for Disease Control and Prevention, and the Georgia Department of Human Resources. At its creation in 1981, to address the high rates of infant mortality in the state of Georgia (United States), the Center was asked by the World Health Organization (Geneva) to be one of its four global resource centers in reproductive health and perinatal care. It has participated in projects to improve reproductive outcomes in over twenty countries worldwide. The mission of the Center is to “serve the people who serve the people” (McCarthy B. and Brann A. Vision and Mission Statement, World Health Organization Collaborating Center in Reproductive Health [currently, the Global Collaborating Center in Reproductive Health], 1992, 2002, 2010). At the invitation of a country’s Ministry of Health, the Center provides the foundation of knowledge and skills necessary to do health services research, which then enables health professionals and other decision makers to sustain autonomous efforts to accomplish the goal of a healthy and wanted pregnancy with the best possible outcomes for the mother and baby.
Former Russian President Vladimir Putin stated in his annual address to the federal assembly in May 2006, “What is most important for our country?…. The most acute problem facing our country today—the demographic problem…. we need to increase the birth rate” (Putin 2006). This demographic crisis is profoundly and adversely affecting the country, its families, its economic competitiveness, and its national security. The two major contributors to this crisis are a short life expectancy and birth rates below replacement level. The life expectancy for the Russian man in 2008 was 59 years, and for the woman, 73 years (IndexMundi, Russian Life Expectancy at Birth 2008). Similarly, the estimated fertility rate for Russian women in 2008 was 1.4 births per woman (IndexMundi, Russian Birth Rate 2008). This is far below the fertility rate of 2.1 births per woman, the figure generally accepted as the fertility rate necessary to maintain a stable population. The low fertility rate and higher and earlier than expected death rate equates to the loss of some 590,000 people per year. This demographic crisis is unprecedented for a major world power, absent war or a national disaster.
Efficacious programs to increase life expectancy depend on adult behavioral changes across the entire life-span of the adult—generally a slow process. Programs to increase the number of surviving normal newborns can make an immediate and long-term impact on this decline. In Russia, both approaches must be undertaken. In order to be successful, the programs must address both the behavioral and social context of disease and the health services for men, women and children through their lifespan.
The Moscow Oblast, with a population of over 7.6 million, is the geopolitical area of Russia that surrounds the central federal district of Moscow City. Roughly the size of the state of Georgia, the Moscow Oblast has a significant number of medically under-served urban and rural populations. Since 2001, General Boris Gromov, the Moscow Oblast Governor, understanding the significance and urgency of the demographic crisis, has allocated significant funds to focus on improving reproductive outcomes. Briefly, the Center Balashikha Project began in 2001 when Governor Gromov and the Ministry of Health invited the Future of Russia Foundation (FOR) to initiate a maternity project in the Moscow Oblast. Following FOR’s initial vision, the Balashikha Project and its goal were jointly developed in association with Dr. Alfred W. Brann, Jr., the Director of the Center, when he was asked to become the project’s medical director. The Project’s goal was to convert the Maternity House in Balashikha into the Moscow Region Perinatal Center (MRPC)—a modern regional perinatal center using internationally accepted standards of care—to provide: (a) specialized perinatal care for both high risk mothers and newborn infants; and (b) postgraduate education in evidence-based practices for reproductive health and perinatal care for perinatal health professionals from all maternity centers throughout the Moscow Oblast. The Project has been successful in achieving this goal.
Over the past 6 years, the success of the Balashikha Project has been evidenced by the increased numbers of women electing to deliver in the Balashikha Center (from 900 to over 3,000 deliveries); by the referral of high-risk women from over half of the Moscow Oblast’s other health districts; by the fact that all post-graduate education for perinatal health professionals in the Moscow Oblast now occurs in the Balashikha center; and by the fact that in 2008 President Medvedev, before he became president, visited the center and stated that he wanted to use this hospital as a model for a modern perinatal referral system throughout Russia, with over 20 similar hospitals being proposed to facilitate development of this system (Emory University Office of International Affairs 2008).
Work on the Balashikha Project has resulted not only in improved healthcare for Russian women and their babies, but in a strong relationship of trust between FOR and the Center staff and their Moscow Oblast partners. Discussions of American and Russian culture and health care have gone on, including an open sharing of thoughts on medical professionalism; clinical ethics, especially end-of-life care; and research ethics using human subjects. Discussions of new and different approaches to a variety of problems frequently seen in modern neonatal/perinatal centers have been possible through the strong trust relationships that have been developed during this project. It is this open communication and trust relationship that has allowed the Center staff to gain the insights into the Russian health care system that allowed us to ask the questions, and to elicit the open answers, that formed the basis for developing the Center’s First International Ethics Conference.
Concept Development of the First International Ethics Conference
Between 2001 and 2005, the FOR and the Center worked intensively on a number of initiatives with the healthcare professionals in converting the Balashikha Maternity Center to the Moscow Region Perinatal Center. Specifically, the first tasks were to: (a) develop accurate data acquisition and statistical modeling; (b) provide lectures and information necessary to develop protocol such that modern perinatal and neonatal health care could be delivered; and (c) suggest changes in facility, equipment and personnel so that the care in the Balashikha Maternity Center would be comparable to that delivered in similar centers in other modern industrialized nations. It rapidly became apparent during these early years that a significant question raised by the MRPC physicians was not only what to do in a specific medical emergency, but “If you can do it, should you?” The issue of ethics of care for the mother and baby had to be addressed.
In the United States, the Neonatal Resuscitation Program (NRP) has for over two decades been the basis for the standardized approach to neonatal resuscitation. Endorsed by both the American Heart Association and the American Academy of Pediatrics as well as a host of other American and Canadian professional associations, the NRP has been required as an educational prerequisite in virtually all north American medical schools, pediatric training programs and neonatal centers. It has provided consistency and focus to a recognized area of extraordinary health risk. [Note that the rate of infant deaths under 1 year of age is greater than the rate of deaths for any decade until the age of 60–69 years (Center for Disease Control, Prevention 2008, p. 21). In the 2006 Textbook of Neonatal Resuscitation, fifth edition, several significant statements are made: (1) “There is no United States federal law mandating delivery room resuscitation in all circumstances.” (2) “In most circumstances, it is ethically and legally acceptable to withhold or withdraw resuscitation efforts if the parents and health professionals agree that further medical intervention would be futile, would merely prolong dying, or would not offer sufficient benefit to justify the burdens imposed.” (3) “Examples of situations where the risk of almost certain early death, and unacceptably high morbidity is likely among the rare survivors, resuscitation is not indicated, although exceptions may be appropriate in specific cases to comply with parental request. Examples may include the following: Newborns with a confirmed gestational age of less that 23 weeks or a birth weight of less than 400 grams; anencephaly; confirmed Trisomy 13 or Trisomy 18 syndrome.” (Kattwinkel 2006, 9-5).
The Russian physician generally takes on a paternalistic responsibility for the care of his or her patients within the scope of the law as prescribed by the state. Frequently in discussions of care guidelines, our Russian obstetrical and neonatal colleagues referred to protocols for care defined by the state in a “white book.” These care guidelines are apparently written centrally and define the legal obligations of care and what is clinically mandated in specific situations. The national professional organizations, when they exist, are generally neither as strongly organized nor have the authority to promulgate guidelines for care or for ethics as their various American counterparts are and do. There is some concern that because of the lack of availability of Western evidence-based healthcare literature, the Russian healthcare system was somewhat isolated and not able to participate in recent medical advances—especially pharmacological innovation (Marquez et al. 2007). Thus, the Russian physician is simultaneously subject to a centrally defined law but, in the case of an individual patient, obligated to care for the patient and in a system where the “best care” may not be based on the same evidence-based protocols that can be found in Western Europe. This conundrum presents a significant challenge and risk to the physician responsible for the care of an infant on the edge of viability.
In the case of the baby born at the edge of viability, Russian law apparently mandates aggressive physiologic support after care has been started. The role of the parents in helping to decide care direction if their baby is potentially severely damaged is not completely clear. In discussions with our Russian colleagues, it appears that the physician, not the parent, is almost solely responsible for the care decisions. However, the parents will certainly be responsible for the economic, emotional and practical care responsibilities of the damaged baby. Additionally, enormous use of scarce resources might be required unless there is discussion of how best to manage this situation. As a consequence of this tension, the Center decided to sponsor a conference to explore with a group of international neonatologists, the approach to difficult clinical situations where the management was significantly impacted by the ethical dimension of provision or withdrawal of life sustaining treatment.
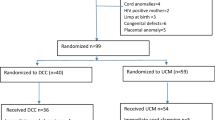
The first international ethics conference was held in Gothenburg, Sweden in October 2006. Neonatologists representing the countries of Russia, Sweden, Norway, the Czech Republic and the United States were present. A total of approximately 40 neonatologists were present. The Russian neonatologists were all physicians working as fellows within the Balashikha Center. The representative from the Czech Republic was asked to participate because their system of health care was subject to the old Soviet dictums, but was able to emerge in the mid-1990s with a neonatal care system that was comparable to those in Western Europe and the United States. The Scandinavians were asked to participate, because their neonatal care systems have long been recognized as having some of the best outcomes in the world. A total of approximately 40 neonatologists were present: three from Russia, three from the US, one from the Czech Republic, eight from Norway and approximately 25 from Sweden. One presenter was selected by each country to speak for that country.
Three difficult cases were presented to these neonatologists. The cases were those of an extremely immature infant, a baby with severe hypoxic-ischemic encephalopathy, and an infant with 18 Trisomy. Only the case and discussion of the extremely immature infant will be presented here. The format for the case discussion was the following: (1) The facts of the hypothetical case were presented. (2) The representative selected from each country presented the usual resuscitation modality. (3) Following the discussion of resuscitation modalities, each country representative would have a brief time (5–10 min) to talk about his or her approach to the infant following resuscitation. (4) Subsequently, there was open discussion with comments from the other international conference participants. It is important to note that even within each country the approach may be highly dependent on the center and philosophy of the neonatology group involved. Thus, the reported specific practices reflect the practice of individuals from each country and not necessarily the practices of that country.
Hypothetical Case Presentation
“Ms. B presents to the obstetrical service with frank rupture of amniotic membranes at 23 4/7 weeks. She is admitted to the hospital and treated with usual hospital protocols for a woman at this gestational age. Two days later, at 23 6/7 weeks, she begins to have contractions with progressive dilatation of the cervix. By the next morning, delivery is imminent. As the neonatologist working that morning, you are called by obstetrics about the delivery.”
International Discussion
Russia
Steroids would be given to the mother if amniotic membranes were intact. Antibiotics would be given to the mother as a routine. A neonatologist would be present at delivery. “Usual” resuscitation would be administered. (It should be noted that there was no discussion of what constituted “usual.”) Ventilatory support would be offered, the infant would be assessed hourly, and fluids would be given as appropriate.
Czech Republic
Prior to delivery, the mother would be transported to a perinatal center experienced in dealing with infants at this gestational age. Steroids and antibiotics would be given to the mother irrespective of rupture of the membranes. The obstetricians and neonatologists would confer on whether to do a Caesarean delivery for an infant of this size, and would discuss their recommendation with the parents. Caesarean delivery may or may not be indicated, but was frequently used if there was a possibility of a viable infant. The data from the Institute for Mother and Child in Prague indicated that over 80% of infants born at 24 weeks or more survived; however, in 2006, they never attempted resuscitation below 24 weeks. The infant would be assessed at delivery because of the variability in gestational assessment; following the assessment the neonatologist would talk to the parents and give them the infant’s gestational age. If the infant was less than 24 weeks and with the parents’ understanding, aggressive care would not be offered. (That is, the infant would be allowed to die.)
Norway
Norwegian neonatologists would talk to the parents about their wishes for the infant and then respect the parents’ wishes. The inference seemed to be that most parents would not want resuscitation for their baby. If, however, the parents did want resuscitation, and if the baby was breathing, then the neonatologist would intubate and resuscitate. Again, the inference was that if the infant was not breathing, resuscitation would not be undertaken even if the parents wished this intervention. One critical feature of the resuscitation was for the neonatologist to do an assessment of gestational age since the obstetricians were felt not to be extremely accurate with their assessments. Thus, an infant thought to be 23 plus weeks, might be 25 or 26 weeks—and vice versa. For this reason a neonatologist must be in the delivery room at the birth of every infant with potential marginal viability. Resuscitation would not be undertaken if the baby was too immature or if the parents did not wish this.
If, following the delivery, the infant was resuscitated, the infant would be reassessed over the next 12 h—specifically a cranial ultrasound would be done at 12 h of age. If an intracranial hemorrhage were present then withdrawal of care would be discussed with colleagues and with the parents. If there was no bleeding, then care would continue.
The infant would be resuscitated initially and an ultrasound would immediately be done in the intensive care unit. The presenter noted that they were not looking for intraventricular hemorrhage, which he felt was overrated, but rather they were looking for evidence of pre-delivery cysts or other types of cysts and perinatal damage.
United States
The approach in the United States is very similar to that used in the Czech Republic. Specifically, the neonatologist would talk to the parents and would present the outcome statistics of infants at that gestational age. As outlined from the other countries, the approach is highly dependent on the center and philosophy of the neonatology group. However, neonatologists from the United States centers represented (Emory University and the University of Oklahoma) would resuscitate at 24 weeks, and would not resuscitate at 22 weeks. At 23 weeks the approach is usually to assess the situation individually.
Withdrawal of ventilation is appropriate if the infant has a major intracranial bleed. But withdrawal of care is one of the most difficult situations. If the parents insist on aggressive resuscitation, then a discussion of the parents’ long term goals for their child might be raised so that if the infant’s situations were to change, then these goals could be used to signal a change in care plan should the infant deteriorate. The option to stop life support, including the ventilator, and allow the baby to die remains an option even after initial resuscitation.
Sweden
Gestational dating is routine at 16–18 weeks of gestation so dating of the pregnancy is generally good. The approach has changed significantly over the past year. The approach in 2006 was that infants would be transferred in utero at 23 weeks. Previously, this transfer took place at 24 weeks and above. It was noted that there was a distinct geographic difference between neonatologists in northern and southern Sweden. Generally, it was felt that the northern neonatologists were more aggressive with intervention. A neonatologist would be in the delivery room, but there was felt to be much variability in the approach by both region and hospital. Resuscitation would usually be with continuous positive airway pressure alone and not necessarily with intubation. This was done to allow the baby to establish his own functional residual capacity without the potential damage from positive pressure ventilation. If the baby is breathing on his own after 10–15 min, then the infant would be intubated and given surfactant. The neonatologist would talk to the parents, but generally the infant would be aggressively resuscitated. Most of the neonatologists would not stop care even at the parents’ request. This was especially true if the baby was on continuous positive airway pressure and not needing ventilatory support.
Open Discussion Regarding the Medical and Ethical Aspects of Care
One of the critical factors in deciding whether the very tiny baby is viable has to do with its gestational age. Conference participants enumerated a number of physical signs of immaturity that would influence them not to resuscitate (Table 1). Although these signs are apparently objective, there is enough subjectivity in evaluating each one, especially following delivery when rapid decisions about resuscitation must be made, as to make the evaluation of these signs a concern. It might be considered best to have an objective measure available when life and death decisions are being made.
There were significant medical and ethical concerns about the decision of whether to do a Caesarean delivery for infants of this gestation age. In Sweden, their data shows an improved outcome in tiny babies born by Caesarean delivery; therefore, one frequent question discussed at the time of birth was whether the neonatologist should try to influence the obstetrician. Discussants from other countries felt that there was no good data in their country or nursery to indicate improved outcome so such a discussion was not useful. Caesarean delivery was, however, frequently used because of breech positioning. The discussion was unclear if the Caesarean delivery in this circumstance was to improve the chances of survival of the infant or if the concern was the health of the mother if the infant became “stuck” in the birth canal and had to be forcefully removed.
Another significant issue for neonatologists is whether they would opt not to resuscitate an infant born after a Cesarean delivery because the infant was judged to be too immature to survive. The general feeling was that the decision to do the Cesarean section was frequently an obstetrical decision based on the information available, but that the decision to resuscitate was a neonatology decision predicated on more complete information about the physical appearance, degree of immaturity, and responsiveness of the newly born baby. Thus, respondents from Norway, Sweden and the United States stated that they would not feel obligated to resuscitate in this situation, but that this was an extremely difficult situation. Therefore, the obstetrician and neonatologist must work closely together and communicate this potential outcome to the parents.
The extent of the resuscitation also became an issue of discussion. Scandinavian participants were undecided about the efficacy of resuscitation of the extremely immature infants. They asked what was done in the United States. The United States respondents all felt that data seemed to indicate that babies who required very aggressive resuscitation would generally not survive or would do poorly anyway, so medications like epinephrine were frequently not used at this gestational age. While epinephrine in resuscitation is generally accepted as a standard, its use would be potentially contraindicated if the outcome following its use was dismal.
A number of the neonatologists from Sweden were concerned that if a baby who was in the intensive care unit, but who was virtually certainly going to die, survived for days or several weeks, then the care of such an infant might inflict pain or suffering; therefore, the babies were routinely treated for pain. While the United States might use pain medications (e.g., morphine) in such infants, it was used more specifically for procedures rather than prescribed as a routine.
Neuro-developmental outcome of the very tiny baby has always been a concern of neonatologists and parents. The Russian participants stated that their data showed that there was a 60% chance of death with the remaining infants universally having a poor quality of life. While this poor quality of life was not defined, the impression left by the Russian neonatologist is that this would include such diagnosis as mental retardation and cerebral palsy. This comment seemed to infer that even though resuscitation might be done in the delivery room (as noted above) that because of the universally poor outcome, Russian neonatologists might not be as aggressive about maintaining the infant in the NICU. Swedish neonatologists noted that if there was no intraventricular hemorrhage or chronic lung disease, the development could be good. However, they noted that this perception was anecdotal and that a better predictive system was needed. One of the United States participants noted that both boys and girls were resuscitated equally, although some data would indicate that girls had better neuro-developmental outcomes.
The availability of equipment was a shared problem between Sweden and Russia. Ventilators were noted to be in limited supply so that neonatologists in both countries wanted to be sure that a baby has a good chance for living before being placed on the ventilator. Additionally, from the experience of the Center in Balashikha, the neonatologist had personally to do most of the care which might be done by respiratory therapists or trained nurses in other countries. Thus, the personnel limitations for ongoing intensive care could present a challenge for our Russian colleagues.
Withdrawal of life support, most especially the withdrawal of ventilation, was a topic that created much discussion in the group. Obviously, it was an ongoing concern for neonatologists in all of the countries represented. Swedish neonatologists noted that the only way to be certain that a baby is viable is to give it every chance and then withdraw care if the outcome seemed poor. Scandinavian neonatologists generally felt that if, after a period of observation, death or “bad outcome” was inevitable, withdrawal of care is an option. They also noted that this is something that was not talked about in public, so that there was not broad public or even professional consensus about withdrawing care in such situations. Both Swedish and Norwegian neonatologists indicated that the decision to withdraw care would be one made after a period of observation and assessment. Thus, the Scandinavian neonatologist must be able to start care and then stop if the outcome appears dismal. This approach is distinctly different from countries where withdrawal of care is not condoned culturally or legally. The Czech Republic and Russia have laws that prohibit the withdrawal of care. Therefore, in these countries, if care has already begun and a baby is assessed as having a poor chance of survival, they continue care without increasing the intensity of care if the infant were to become ill. Thus death occurs, but without overtly stopping care. The approach in the United States is generally similar to the approach in Scandinavia, that is, the withdrawal of life support after a period of observation. It was noted, however, that “care” is never stopped—only the highly technical life support. Specifically, management of pain and suffering, warmth and nursing support is provided as part of “caring” at the end of life. In the United States, this approach is often referred to as “comfort care” to indicate that the primary purpose of the care is no longer life-saving but comfort-giving.
There was concern expressed that there were not uniform guidelines (such as the NRP provides) for resuscitation or for the ethics of care. A lengthy discussion ensued about the variability of approaches to resuscitation. The International Liaison Committee on Resuscitation (ILCOR) of the European Resuscitation Council is an international interdisciplinary group with the purpose of providing a forum for discussion of resuscitation principles. One of the objectives of ILCOR is to produce statements on specific areas of resuscitation that reflect international consensus. The 2005 ILCOR guidelines are virtually identical to the United States NRP statements:
When gestation, birth weight, or congenital anomalies are associated with almost certain early death and an unacceptably high morbidity is likely among the rare survivors, resuscitation is not indicated. In conditions associated with a high rate of survival and acceptable morbidity, resuscitation is nearly always indicated. In conditions associated with uncertain prognosis, when there is borderline survival and a relatively high rate of morbidity, and where the burden to the child is high, the parents’ views on starting resuscitation should be supported. If there are no signs of life after 10 min of continuous and adequate resuscitative efforts, it may be justifiable to stop resuscitation (American Heart Association 2005, p. III-96).
However, these specific recommendations were modified in respect for the international variability which was recognized by all participants by stating that these “guidelines must be interpreted according to current regional outcomes and societal principles” (American Heart Association 2005, p. III-96).
Despite the potential for consensus, the participants in this 2006 international conference sponsored by the Center noted that guidelines for resuscitating infants were inconsistent even within a country and frequently were hospital specific. It was noted that for many of the participants, the ethics of care was infrequently talked about even in private, and that virtually no conferences on the ethics of care were available where professionals could talk about the issues raised at this conference. They seemed truly appreciative for the opportunity. Thus, the lack of consistency of the medical, much less the ethical, components of resuscitation makes it essential for physicians to begin to talk among themselves and with their patients.
References
American Heart Association. (2005). Part 7: Neonatal resuscitation. Circulation, 112 (22_suppl), III-91-99.
Center for Disease Control, Prevention. (2008). National vital statistics report. Atlanta: Centers for Disease Control and Prevention.
Emory University Office of International Affairs. (2008). Key international accomplishments in 2007–08: Emory, Europe and Eurasia [On-line] available from: http://www.international.emory.edu/sub-news-EUeurope.htm. Accessed 8 April 2009.
IndexMundi (2008). Russia Birth Rate. [On-line] available from: http://indexmundi.com/russia/birth_rate.html. Accessed 23 March 2009.
IndexMundi. (2008). Russian life expectancy at birth. [On-line] available from: http://indexmundi.com/russia/life_expectancy_at_birth.html. Accessed 23 March 2009.
Kattwinkel, J. (Ed.). (2006). Textbook of neonatal resuscitation (5th ed.). Elk Grove Village, Il: American Academy of Pediatrics, American Heart Association.
Marquez, P., Suhrcke, M., McKee, M., & Rocco, L. (2007). Adult health in the Russian Federation: More than just a health problem. Health Affairs, Countries Studies, 26(4), 1040–1051.
Putin, V. (2006). Annual address to the federal assembly. Moscow: The Kremlin.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sexson, W.R., Cruze, D.K., Escobedo, M.B. et al. Report of an International Conference on the Medical and Ethical Management of the Neonate at the Edge of Viability: A Review of Approaches from Five Countries. HEC Forum 23, 31–42 (2011). https://doi.org/10.1007/s10730-011-9149-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10730-011-9149-6