Abstract
Background
Transcranial direct current stimulation (tDCS) is a brain stimulation technique currently being researched as an alternative or complimentary treatment for various neurological disorders. There is little knowledge about experiences of the participants of tDCS clinical research, especially from pediatric studies.
Methods
An interview study with typically developing minors (n = 19, mean age 13,66 years) participating in a tDCS study, and their parents (n = 18) was conducted to explore their views and experiences and inform the ethical analysis.
Results
Children (10–13 years old) and adolescents (14–18 years old) reported good experiences with the stimulation. Next to financial incentives, main motives to participate in the study were curiosity and the possibility to help develop treatments for children affected by neurological disorders. They could also see a potential of using tDCS in a non-medical setting, especially regarding the provision of equal opportunity, e.g. in education. Parents also presented a positive attitude towards tDCS and their children participation in the basic research study. Nevertheless, their understanding of tDCS was rather poor. Even though many of them understood the techniques, they often did not see the link between the (current) lack of side effects and an absence of longitudinal studies. Parents were also cautious about using tDCS for non-medical/enhancement purposes.
Conclusions
The study findings show a need for more transparent information about the state of the art of tDCS, its function and what it might be able to offer, especially considering the good acceptability of tDCS.
Similar content being viewed by others
Introduction
Transcranial direct current stimulation (tDCS) is a non-invasive brain stimulation technique involving the application of a weak constant direct current between head-mounted electrodes. Due to the transcranial application, a large part of the current is conducted through the skin, skull and the cerebrospinal fluid (CSF), while a small portion actually reaches the brain [1] (for review see [2]). Because of these low current levels in the brain, tDCS does not trigger action potentials [3]. Instead it is assumed that the induced E-field in the brain leads to a polarisation of the neuronal membranes and thus influences the endogenous neuronal activity. tDCS effects are not uniform, but appear to be influenced by a variety of methodological and physiological factors [4, 5].
tDCS is categorized as a non-invasive transcranial brain stimulation, in contrast to, for example, deep brain stimulation, which is performed under general anesthesia [6]. Due to its relatively easy application and apparent lack of severe side effects, tDCS is considered a promising intervention for various neurological disorders, e.g. schizophrenia [7], attention deficit hyperactivity disorder (ADHD) [8]. In depression [9], and various pain conditions [2] the technique has already proved effective. It should be noted, however, that tDCS has proved more effective in the acute depression rather than in long-term (and treatment resistant) depression and its efficacy might depend on other treatments that are used simultaneously [10]. Despite an increasingly broad spectrum of research, there are still several uncertainties around tDCS that need to be addressed before it can be successfully translated into clinical practice. Although levels of evidence for tDCS of various conditions have been assessed as rather high [11], establishing the tDCS’ parameters that would have reliable behavioral impact is a pressing research need, as well as gaining full understanding of neurophysiological mechanics [12].
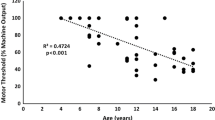
The application of tDCS to pediatric populations has been increasing rapidly, nevertheless this population continues to be underrepresented in comparison to adults [13, 14] and there remains a pressing need to investigate the mechanisms, behavioural effects, and safety of tDCS in the developing brain. Unique anatomy and the developmental changes that take place throughout childhood suggest that tDCS effects will vary and differ from adults. For example, the developing brain is thought to have a shifted balance of excitation-inhibition(E:I), resting closer to the seizure-threshold [15]. Since physiology, pharmacology, and anatomy differ between adults and children/adolescents, it cannot be taken for granted that identical stimulation protocols induce the same effects in different age groups [16, 17]. Recently it has been shown that the current density analysis across different age groups indicated the necessity of age-dependent intensity adjustments in tDCS applications for young subjects, to compensate for structural differences due to the growth status [18].
This growing interest in developing tDCS interventions for children is particularly motivated by the side effects associated with the medication currently administered for neurodevelopmental disorders [19] and the relatively easy application of tDCS [13]. Although it is considered a fairly safe technique, some concerns have been raised regarding the use of tDCS on the developing brain [20]. These worries and reservations are linked to several unknowns in relation to tDCS, in particular, the lack of long-term evidence regarding potential damage to the brain and cognitive as well as emotional function, insights regarding potential interaction between environmental and social factors and tDCS, and a lack of ununified study designs [20, 21]. The only way to address those unknowns is to conduct more tDCS research in pediatric populations [14]. This research is needed in both therapeutic areas and as well in typically developing cohorts to better understand the mechanism underlying the technique.
Brain structure and function are abnormal in neurodevelopmental disorders. Therefore, to further investigate tDCS parameters in pediatric populations, typically developing children and adolescents also must be included in research. They serve as a reference population and their participation helps to establish the margin of improvement that can potentially be achieved in active groups (e.g. in clinical studies with children and adolescents with ADHD) [22]. The primary principles of tDCS effects in the developing brain have not been fully defined yet. Hence, it is essential to conduct research in typically developing cohorts of pediatric tDCS to determine safety, tolerability, and effects on motor learning in typically developing children [23,24,25]. Usually in research, there is no direct benefit for the study participants in the healthy control group. In the case of typically developing groups in tDCS research, this might be different, particularly considering the possibility to learn more about the functioning of one’s brain, and also in light of expectations that tDCS might ‘enhance’ the functions of a typically developing brain [25]. The stimulation settings might be also different for enhancing purposes compared to the treatment of an atypical brain [26].
These various uncertainties notwithstanding, the number of clinical studies examining the effects of tDCS is increasing [27],Footnote 1 however a review of the top 100 cited tDCS and TMS trials between 2008 and 2017 concluded that most of the cited trials are small feasibility studies and in order to establish clinical effectiveness, more robust clinical trials are needed [28]. Furthermore, since children and adolescents are a vulnerable research group [29], data for this population are rather limited. Also, the focus has hitherto been on the analysis of clinical data, mostly from the patient group and little is known about typically developing participants’ knowledge and experiences of tDCS. The importance of taking into account potential patients’ voices has been recognized in clinical research [30]. It can be argued that the views and perspectives from typically developing cohorts, and in case of tDCS also potential users, might contribute to a more responsible integration and a more effective translation into clinical practice. Translational research is also based in providing information on needed behavioral change, helping to make more informed choices, and ensuring that new treatments and knowledge reach the appropriate population [31]. Typically developing tDCS participants are more likely to participate in research without high expectations or wishes, hence the risk of, e.g., therapeutic bias is smaller, and their observations and experience are valuable for further assessment of the technique. In addition, because a typical brain might react differently to stimulation then an atypical one, balancing risks and benefits might therefore be different for typically developing children and minors in tDCS studies than in pharmacological trials.
Interest in tDCS as a “do-it-yourself” (DIY) application [32] and using commercial devices is also present among the broader public, in relation to both treatment and as a form of neuroenhancement [33]. Regulatory frameworks are different across various countries and the status of tDCS in clinical settings [34] and as a direct-to-consumer application [35] has not been fully regulated everywhere. In the USA tDCS devices are allowed at the market (as “FDA cleared”), however they have not been cleared for marketing as a medical device [36]. In other countries, regulations are limited to particular disorders, e.g. as a complementary treatment for major depression in the EU and UK [37], or for chronic pain in Canada [38]. Although there are no official guidelines in other areas (especially for use by children and adolescent populations), tDCS devices can be easily purchased online. With the increasing number of tDCS studies, also among pediatric populations [14], and with the relatively easy access to commercial or DIY tDCS devices, it is important that the ethical issues with regard to non-clinical use are also addressed promptly.
This paper aims to contribute to closing the research gap by exploring first-hand narratives in typically developing children and adolescents participating in the tDCS study. It reports on findings from an interview study conducted among typically developing children and adolescents undergoing tDCS and their parents. The study aimed to explore their views, experiences, and expectations of tDCS. Furthermore, it focused on motivations to study participation from the perspective of participants from the typically developing cohort. Views on enhancement and non-clinical use were also discussed. An exploration of the understanding of tDCS among study participants, their perspectives on tDCS, views on non-clinical applications, and understanding of potential risks can provide a basis for the adequate implementation of tDCS in clinical practice. Reflection on these issues is also essential to avoid unnecessary hype or anxiety regarding the technique. The study participants’ personal narratives are important elements in providing a robust research picture of the effects of tDCS.
Methods
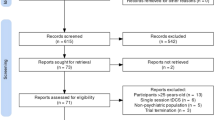
This was a semi-structured, qualitative interview study [39]. Interview study was chosen as a best method to capture perspective, values, and experiences of tDCS among pediatric population and their parents. It enabled focus on the aspects of tDCS that are usually not collected or investigated in statistical and clinical analysis- such as personal experiences, meanings, worries and motivations. The study was approved by the local ethics committee (University Medical Center Schleswig Holstein D 449/17). The development of the topic guide was based on an extensive literature review [13, 20, 24, 33, 34, 40,41,42,43,44,45,46,47,48,49] and discussed within the research team. The topic guide was tailored appropriately to children [10–13] or adolescents [14–18] age and pretested [50] in the piloting phase, which involved five interviews with children and parents from another tDCS control group study, and questions that proved redundant were removed. Participants were recruited from the study “Optimize parameters for effective stimulation based on individual modeling”( OptiStim study). The interviewer did not know the participants prior to the interview study. Participants and their parents received a detailed introduction to and explanation of tDCS while signing the informed consent (or assent) to OptiStim study. Owing to the nature of the interview study and since OptiStim study and the interview study took place within a similar timeframe, no repeated introduction to tDCS or further information about the technique were given prior to the interview. However, participants were invited to ask any questions they might have about the technology.
Description of the OptiStim Study from Which Participants were Recruited
The OptiStim Study (DRKS00008207) is part of the H2020-funded STIPED research consortium (“Stimulation in Pediatrics”, www.stiped.eu), which aims to optimize parameters for effective brain stimulation in children and adolescents. This study investigated the effects of anodal tDCS (vs. sham stimulation) on working memory and response inhibition dependent on concurrent and non-concurrent target tasks during stimulation, taking interindividual factors into account. Based on these results, a pipeline for the application of individualized and optimized stimulation will be developed. The study consisted of two independent, non-overlapping, double-blind, sham-controlled, crossover groups of typically developing participants. Children and adolescents between 10 and 17 years were included in both groups. Participants were excluded in cases of any relevant neurological or psychiatric diseases or psychological symptoms, metallic head implants, regular concomitant medication, substance consumption, and—for female participants—in case of pregnancy. Both groups attended five stimulation sessions, with one additional optional magnetic resonance imaging (MRI) session. At the end of each stimulation session, participants completed a questionnaire on the safety, tolerability, and blinding of stimulation. In the stimulation sessions each participant received four different stimulation conditions in randomised order: twice verum stimulation and twice sham. Sham tDCS acted as a control condition, in which a few seconds of stimulation at the start (ramp up) and the end (ramp down) of the programmed time period was administered to a participant in order to minimize cutaneous perceptions, which are typically reported within the first few moments after the stimulator is turned on [51]. In this study 2 mA tDCS was applied. For verum stimulation current was ramped up for 30 s followed 20 min stimulation and ramped down during 30 s at the end of stimulation. For sham stimulation current was ramped up and immediately down for 60 s at the beginning and end of the stimulation. Participants received up to 60 € for the study participation, 10€ for each completed appointment, irrespectively if they completed the study or not. Additionally travels costs were reimbursed.
Interview Study
The aim of the interview study was to recruit around 20 minors and 20 parents in order to reach data saturation [52].
Since this was a double-blind clinical study, neither the minors participating in the tDCS study (and their parents), nor the interviewer of the present study knew if the interviewed minors have received stimulation or sham-stimulation during a particular session preceding the interview. Children and adolescents and their parents were offered a small financial incentive (a €10 voucher) to participate in the interview study. All interviews were conducted face to face after signing additional informed consent for the interview study by parents and assent form by underage participants. An external audio recorder without connection to the internet was used to record the interview.. The interview with a child/adolescent always took place after the stimulation to prevent potential influences on the stimulated brain and the data [53]. The interviews with the parents were conducted during various stages of the stimulation. Several interviews were conducted prior to the tDCS study, after the parents had received information about the study and had given their informed consent for their children’s participation in the stimulation procedure. Interview study recruitment took place between October 2017 and August 2019.
The interviews with parents lasted approximately 20–30 min. The interviews with children and adolescents were significantly shorter: 6–15 min. With one exception, both interviews were conducted separately; however, children and adolescents were given the option of having a parent present if required. All interviews were led in German by AS, who is trained and experienced in qualitative, in-depth interviews. The quotes below were translated verbatim from German to English, retaining the original grammar, vocabulary, and syntax. The interview guide can be found in the Supplementary Material.
Analysis
Interviews were transcribed verbatim by two student assistants. Six phases of thematic analysis [54] were followed in the analysis. AS recruited and interviewed all participants and coded all the interviews. Codes were identified through an iterative process. After the initial open coding, where texts containing relevant information was labeled with a descriptive tag, transcripts were revisited and reexamined. Eventually, codes were gradually organized into candidate themes, and particular attention was paid to linkages and distinctions between key ideas and concepts and commonalities and discrepancies within and across transcripts. The coding system was both deductive and inductive- initially the codes identified in the literature and presented in the topic guide guided the process of coding (top-down), and during further coding process additional codes were identified (bottom-up). The themes were named with reference to the questions asked in the topic guide. The coding process was carried out in the qualitative coding software MAXQDA 2018 [55].
Results
In total, 37 (19 with children/adolescents, 18 with parents) interviews were conducted. Recruitment for the interview study finished with reaching data saturation when no new information was provided in the interviews [56]. The interviewee age (in case of children and adolescents) is provided after each quotation. The sample description is presented in Table 1. The participant age (in case of children and adolescents) is provided after each quotation.
The findings from the interviews with children/adolescents and parents are presented separately. First, the main themes identified in the interviews with children/adolescents are discussed. Their motivation for participating in the study is presented followed by the themes exploring their experiences of stimulation. In the final section, we briefly discuss children’s/adolescents’ understanding of and attitudes toward cognitive enhancement and tDCS, noting, however, the problematic validity of the discussion of moral issues by minors, particularly in this study in which the age span was quite broad. In the interviews they point to several important issues regarding access and use of tDCS for non-medical purposes, e.g. fairness. However, it should be noted that their young age and lack of experience might have impeded their ability to fully grasp moral concepts or identify more ethical issues. This lack of more in-depth ethical reflection might be also related to the interview itself. Although special attention was paid to develop an age-appropriate topic guide, maybe others form of data collection could even better elucidate the moral discussion with this group.
Participants and their parents received a detailed introduction to and explanation of tDCS while signing the informed consent (or assent) to OptiStim study. Owing to the nature of the interview study and since OptiStim study and the interview study took place within a similar timeframe, no repeated introduction to tDCS or further information about the technique were given prior to the interview. However, participants were invited to ask any questions they might have about the technology.
Findings from the Interviews with Children and Adolescents
Motivation for Participation in Research
Children/adolescents participating in the study were aged between 10 and 17 years. The interviews were relatively short, lasting between 6 and 15 min. The children’s/adolescents’ insights, although limited, are important, as they represent first-hand reports on pediatric tDCS stimulation. In keeping with the tenets of qualitative research, the emergent themes are presented in the discussion that follows and no quantitative conclusions will be drawn. Children/adolescents participating in the research study reported relatively positive experiences of the stimulation. Although many of the participants’ parents were convinced that their children’s main motivation for participation was driven by self-interest, namely the financial incentive, the children/adolescents seemed to understand the importance of their contribution to science and that they might be helping other children in need. While discussing their motivation for participating in the study, most children/adolescent participants did indeed mention the financial incentive; however, that was rarely their only reason for participating. Some children/adolescents were simply curious and wanted to gain new experiences. Some were encouraged by their friends who also participated in the study:
-
““A friend told me [about] that and suggested: that I should take part, too. And then I read it through, and it was interesting, and I thought to myself, why not?” ST17” (17)
Some were simply excited about participating in research and wanted to gain some new experiences:
-
“Hm, I would say that I could get some new experiences this way. That is why I [thought I] would participate and see how it is and if I can yet learn something or so.” ST7 (17)
During the process of gaining informed consent for the study, the participants were informed about the study’s overarching aim and about other research exploring tDCS for various pediatric disorders, including ADHD. This seemed to be important for many, and they viewed their participation as a chance to help others:
-
“Uh… because I just want to support [other] people, that is just something that connects me with society and I’m also helping so that things can go better.” STS6 (17)
Another identified factor that might have influenced decision-making regarding participation in the study was previous experiences with clinical research:
-
“I was contacted, and I was told that first of all it will help other children if the results turn out right. And of course, because of the money, doing that, probably everybody would. I have also participated in several studies, so I know how it works, and I want to work for my money.” STS9 (13)
Experiences of tDCS
Children’s’ and adolescents’ excitement and curiosity about research that were expressed while talking about their motivation were only partially reflected in their responses about the experience of stimulation and its potential effects.
They reported initial pain and itching on the spots where the electrodes had been placed:
-
“Well, it’s just that you feel a little, you know, a little pain (…), but just a little pain in the area where the electrodes are.” STS1 (12)
Regarding the effects of the stimulation and potential changes in concentration and other mental activities, the prevailing response was tiredness:
-
“So, last time I did it, I was very tired afterwards. (…); I could have possibly done another task like that, and then I would get sleepy. But I always had it that way, that I was just medium to wide awake at first and then I got a bit sleepier towards the end.” ST17 (17)
The tiredness may also be attributed to the fact that most stimulation appointments took place during the week, after school. However, fatigue will be investigated in the analysis of the clinical data.
Some children/adolescents expressed excitement about the study; others initially had some worries that dissipated after their initial conversation with the research team or over the course of the stimulation.
Children’s and Adolescents’ Understanding of and Views on Enhancement
The final element of the children’s and adolescents’ interviews was the exploration of their understanding of and views on enhancement. Participants were asked some generic questions about the use of tDCS for non-medical purposes, including what they thought about it generally and, more specifically, how they would assess the fairness of using a tDCS device to improve learning performance or concentration.
Generally, children and adolescents were open to the use of tDCS in healthy people; however, some stated that it should only be available under certain conditions, for instance, to provide more equal chances:
-
“Well, it always depends on the person, if he doesn’t need so much help now, for example, because he can concentrate quite well, I would say that it was unnecessary to do that. But if there are also people who don't have a disorder, but still can’t concentrate well because they are distracted by all kinds of things, then it makes sense to do this so that they can concentrate exclusively on one thing” ST17 (17)
Another adolescent noticed the possibility of side effects and potential implications for autonomy if one were to become over-reliant on the brain stimulation device:
-
“I guess that can also have side effects or I could rely too much on having this stimulation and not do as much on my own” P20T (14)
Several interviewed minors find the idea of using tDCS for the sake of enhancement undesirable. One child expressed a view that the use of tDCS in healthy children without any psychological or cognitive problems would be redundant:
-
“Mm I don't know, because it is basically developed for children who have problems and if healthy children do that now, who just don't have [those problems] I would find it superfluous” ST10 (12)
Another adolescent noticed that stimulation is not neutral but that it takes time and preparation, and as mentioned before, might have some side effects:
-
“Well, I don't know how useful it is. Of course, if you can increase concentration or something like that, maybe it makes sense, but if you don't really need it, if you can function without it. (…) I don't think you have to treat it, because I think that if you function so well, you don't have to let external influences affect you in such a way that you function even better.I don't think that's necessary, because it's always an effort to do that and it always changes you, it takes time and so on.” ST5 (17)
There were also perspectives from the other end of the spectrum, whereby some participants were convinced that the use of a tDCS device could help them get better grades:
-
“Well, when learning, if I studied at home and wore such a cap” and my brain was stimulated, then I would actually find it really good, if I could concentrate better, because then I would also have better grades and not always be distracted.” ST4 (15)
Many children and adolescents interviewed shared the view that using stimulation for non-medical purposes outside of the clinical context, such as for enhancement purposes, is unnecessary. They also pointed to potential side effects. It should be emphasized, however, that their responses included no in-depth balancing of the risks and benefits of non-medical tDCS use.
Findings – Interviews with Parents
Motivation for Signing up their Children for the tDCS Study and Parental’s Perception on their Children’s’ Motivations
Parents were not active participants in the OptiStim study and did not receive the stimulation. However, since they had to provide informed consent for their children’s participation, they were important agents in the study. A significant number of the parents had previous experience with research studies. While many seemed to understand importance of involving children and adolescents in research, a prevailing motivation and reason for encouraging their children to participate was the financial incentive their children would receive. One of the parents described it quite vividly, as follows:
-
“I asked my children, because the pay was relatively good, but of course it is always a bit of a mixed calculation, expensive house, the children have expensive wishes and, yes and then I asked them if they wanted to earn the money, I would drive them and they thought that was quite good, right now it is so with all of them that they are also glad when it is over, because it is just exhausting, we drive a quarter of an hour here. But I asked them, and they all wanted to do it. They had the dollar signs in their eyes a little bit”. STM16
A recurring factor in the decision as to whether to sign their children up for the study was parents’ familiarity with the clinical context from their experiences with other clinical studies or of being employed in a clinical setting:
-
“Since I am a study nurse myself, I am somewhat familiar with studies, have read through it and am always in favor of supporting research” STM3
The value of research and solidarity aspect were also stressed:
-
“I just think it’s important that the research is supported in this way and he has already participated in one study and this is now the second one he has participated in.“ STM1
Another parent saw the participation in a tDCS study as valuable experience for his child:
-
“Taking part in such a study, (…) certainly brings a bit more self-confidence, because she is alone here, as a fourteen-year-old girl, all alone with strangers, (…) it brings her personal benefit, in any case. And it's certainly an experience to just have a look, she also notices what's been done, (…) So, if she wants to get into the medical field at some point, it's certainly also a story that lets her get a taste of what actually happens, what it means to help people.” STV15
General Perception of tDCS, Expectation, and Worries
Generally, parents had limited knowledge of tDCS prior to the study. However, even after signing their children’s study participation documents, their familiarity with tDCS was relatively scant. For instance, they were unable to describe in greater detail the characteristics of tDCS or its potential risks and side effects. Simultaneously, they expressed high levels of trust in research and the local research team. Their trust and reliance on the research team was also inferred by their relatively few inquiries about potential long-term effects. Only one parent expressed concerns about it. He noted that his son might somehow be affected by the results of the brain stimulation in the future, also as a potential, unexpected, incidental finding that would not have been discovered without the tDCS:
-
“If it can also help F. [child’s name], I don’t know. Also, I was hesitant, it is hard to say if there isn’t anything latent in the background. Although I believe that F. is healthy, but it is not known for sure if there isn’t anything there floating, something not known, like 15–20% [risk].” STV11
Parents presented an overall open attitude to the tDCS, strongly motivated by their trust in the research team. They did not have any specific expectations; only one parent hoped that it might help their child, who was experiencing some problems at school:
-
“Expecting would be a bit much now, but at least the hope is there, yes. (…) Well, he now has problems at school (…), so if there is a lot of noise or something, then he likes to switch off quickly and I think, if maybe a bit of it would help him, although with increasing age reason may play a role, and then it might work a bit better.” STM8
tDCS Versus Medication for Treatment of Neuropediatric Disorders
The parents’ overall positive attitude toward stimulation was also evident when they discussed the potential effects of tDCS in comparison with medication. Although the study focused on children and adolescents without any neuropediatric disorders, most parents had some knowledge about, for example, ADHD and usually expressed rather strong views regarding pharmacological treatment. They saw tDCS as a safe alternative and, unlike medication, as not having any influence on other organs. This is how one of the participants expressed this view:
-
“I believe, that it may be possible, that it [tDCS] would be better, because the drugs have an impact on many organs and on the mental state, eventually it has an impact on the whole body, and a central stimulation, which is targeted at exactly this center that is concerned and which triggers this [problem], that of course would be beneficial.” P20M
A recurring belief was also that unlike medication, tDCS does not have side effects, even when used long-term:
-
“Well, I would expect more from the stimulation than from the drugs, so taking drugs permanently, I rather imagine that there could be side effects.“ STV11
This positive view toward tDCS versus medication was also reflected in parents’ general attitudes toward clinical research. While all of them supported their children’s participation in the tDCS study, many of them said explicitly that they would not allow their children to participate in a pharmacological (drug) study.
Parents’ Views on Enhancement
During their interviews, parents were also confronted with the question of use of tDCS for non-medical purposes. While all interviewed parents were against the use of tDCS in healthy minors, they had mixed views regarding the use of tDCS in adults. While little enthusiasm was expressed, many parents shared the belief that tDCS for non-medical purposes cannot be regulated or banned. Some of them compared it to caffeine or other similar stimulants. Most parents also were unaware about the current debate on (neuro-)enhancement. However, some presented a cautious, more reflective approach:
-
“I think that you can perhaps exaggerate this in the sense of wanting to become better and better, but then harming yourself. But it probably doesn't work out the way I imagine it, that you become so super-duper that you become competition for someone else and that this becomes noticeable at school or at work.“ STM18
Another parent also pointed to the differences in the use of enhancement for children and for adults and the negative results it might have when administered to children of school age:
-
“With adults it’s different, they can decide for themselves if they want to improve their performance with such methods or something like that. I think at school age this will lead to more competition and a gap between children whose parents can afford such methods and children who can’t afford it financially. Difficult, so I wouldn’t recommend it. No.” STV4
Parents’ Attitudes Toward tDCS Home Devices and Commercial tDCS
Some tDCS researchers argue that to function as an effective, accessible treatment in the future, tDCS as a therapy should also be available as a home device, either remotely controlled or with parental control [57]. The research on potential challenges and advantages of home tDCS devices is limited and the interview study offered an opportunity to explore parental views on this. We differentiated between tDCS home devices for potential therapeutic purposes, devices that can be currently purchased online, and DIY devices. In the last two cases, we were also interested in parental general awareness of these devices, which turned out to be low. Parents’ views on home tDCS were mixed, and they expressed several reservations about the introduction of this technique at home rather than engaging in an in-depth exploration of the factors that should be taken into consideration when introducing tDCS in home settings. One emerging view was that there might not be a clear-cut answer as to whether a home stimulation is beneficial and that it should be decided on an individual basis:
-
“I think you must look at this individually. If you have parents who, without meaning it badly, are perhaps a little more simpleminded, where perhaps sometimes it is also so that the far-sightedness or understanding is not there. I believe that it would be difficult to teach these parents how to use it at home, so that it has the right effect.” STM16
According to some parents, the feasibility would depend on the family’s situation and how technically skilled the parents were. Some suggested that people might prefer to do it under supervision. It was also noted that home stimulation should be introduced only when tDCS has been sufficiently researched. The arguments raised in favor of the home stimulation included that those treated would experience a more friendly environment at home and that it might be easier to have regular stimulation rather than time-consuming clinic visits.
-
“It probably also depends on the family environment (i.e., how it is dealt with). As is the case with medication. If you work with responsible people (i.e., if everything is mature and works well and the parents or caregivers are conscientious about how they use it), then you could of course do this at home” STM13
-
“I wouldn't have to say anywhere ‘no, I don't have time, I have to go there first and I have to get my dose again’, I don't have that. I say ‘no, no problem, I'll get the dose two hours later at home in my armchair.’” STV15
All parents were unaware of the possibility of buying tDCS devices online. One parent expressed some concerns that it might trigger the interest of the child participating in the study:
-
“So now I start to think about whether it might be harmful for a child to participate in such a study, because it comes into contact with possibilities. Well, if my son now finds out that (…)—I’m not more awake and fitter now or have more headaches or something, then it’s natural, then there’s no danger, but if he now noticed, oh that’s great, I can think much better and solve the tasks much better, then he sits at home at the computer and looks, can I order something like that on the Internet or watch some YouTube videos, I wouldn’t like that.” STM1Footnote 2
Adverse Effect: Epileptic Incident
During the OptiStim study, an adverse event was recorded: previously undetected epilepsy was diagnosed in one of the study participants following a seizure. Although no causal relationship was detected between tDCS and the seizure (see the clinical case description [58]), this case is an example of a previously unknown neurological illness being revealed through participation in a control group study. Three months after the incident, we invited the participant and her mother for an interview. The topic guide of our interview study was extended with several additional questions exploring the epileptic incident (see published ethical case analysis [59]). Both the participant and the mother had a good experience with the tDCS study and although a causal link between tDCS and the epileptic seizure cannot be confirmed, they acknowledged that the child’s participation in the study might have contributed to a faster diagnosis:
-
“As I said, she had this tremor and this first attack before the stimulation. Without stimulation, it could be that she has such small seizures from time to time, and we would never have known what it was. (…) And without this big seizure, if it had only happened from time to time, that wouldn’t have been nice either, because you don’t know what’s going on. And what I also said before, if a seizure really happened in a dangerous situation, for example if she was in the water or if she was driving a car later and you don’t know that you are ill, then it would be tragic. But with this big seizure, it determined that she has epilepsy. And you just have to be a bit careful with some things. I don’t care whether it was connected with the stimulation or not, the main thing is that we now know what is going on. It was actually good that something like that happened during this time.” (ST19TM)
Discussion
Research studies with healthy volunteers are not planned to benefit the participants, and comprehensive justification must be provided as to why such research involving potential “adverse and serious adverse events” must be performed on them. Overall, we encountered positive attitudes toward tDCS in both children/adolescents and parents. Participants had some strongly pro-social motives to participate in research. A good level of acceptability of tDCS was also discussed in a study with parents of children with ADHD [60]. We also found this in another interview study with the patient group with ADHD and their parents [61] Although this overall positive attitude towards tDCS might make the introduction of tDCS into clinical practice easier, it should not blur the fact that the efficacy might not be the same as with other, currently more evidence-based, treatments.
An unexpected finding was the role of the financial incentive among study participants and especially among several parents. Whereas the prospect of a financial award for study participation is often considered one important motivation factor for research participation [62], its occurrence in the context of our study was different and more worrying. It seemed that the study compensation for some parents was the only motivation to signed up their children for a clinical study. It can be assumed that the adolescent participants might have competence to decide for themselves when it comes to study participation, and voluntariness in study participation was a strong factor mentioned by most of the parents. This might be linked to the fact that there were no clinical expectations related to the stimulation, unlike in the study with children and adolescents with ADHD, where we found that some parents were very motivated for their children to participate in the study, even when the child was less enthusiastic [61]. While children/adolescents should receive some compensation, it might be ethically problematic if their parents were to encourage their participation for this reason alone.Footnote 3 The involvement of typically developing children in a tDCS study is ethically sensitive itself; the ethical justification for it lies in the overall low level of expected side effects and risks, the likely possibility of scientific advances and the fact that without their involvement, the mechanism of tDCS in the developing brains will remain underexplored. This, in turn, would negatively impact the research with children and adolescents affected by neuropediatric disorders. Conversely, while it is remarkable that children/adolescents recognize the importance of their contribution to science by participation in research, it may be worrying that some see it exclusively as a way to earn some extra money. This could undermine the rule of voluntariness in research participants and blur an accurate risk–benefit assessment. Incentives in studies involving children/adolescents are a contested issue [63]; on the other hand, the provision of incentives in the study might have some positive effects of minimizing the risk of therapeutic misconception [64]. The demographic information collected in passing during the interview, e.g. with regard to family income or education level, did not suggest that study participation was motivated by the difficult financial situation, however this issues was not explored directly. The remarkably pro-social motivation in children/adolescents is an important finding. It was present both in the children and adolescent group. Its further exploration might contribute to removing some challenges in recruitment and involving children/adolescents in research.
While studying a cohort of typically developing children and adolescents receiving non-invasive brain stimulation, it seemed suitable to explore their views of enhancement. No enhancing alteration of brain activity was anticipated during the stimulation. Nevertheless, both the children and adolescents as well as their parents were willing to express their opinions on potential influences of tDCS on healthy brain. Many of the views oscillated around understanding tDCS as being an enhancer rather than normalizer [65], which might have impacted their rather reserved position and their perception of tDCS use in healthy people as ethically problematic.
The children’s/adolescents’ views on enhancement provide valuable insights into their understanding of fairness and the improvement of cognitive and other skills. Most of our participants did not support the idea of using tDCS for one’s own benefit, and they believed it should be limited to people who might need it. Even if used with healthy children, they referred only to its use in school, to catch up with missed classes in cases of long-term illness, to be better prepared for tests, or to achieve better grades. This is in line with some of the aspects of the bioethical debate on justice and fairness regarding the social context of neuroenhancement – especially regarding access to neuroenhancement, as well as the blurred lines between concepts of health and disease [66]. In case of tDCS and none invasive brain stimulation methods it has been noted that there are additional ethical challenges that need to be taken into account such as: possibility of an unlimited self-administration, various effects of the stimulation depending on the individual, time of stimulation and other facts, and also the non-detectability of those techniques [67].
The aim of the interview study was not only to illuminate participants’ and their parents’ understanding of potential ethical issues related to tDCS but also to explore their views as active stakeholders in this context. The interviews with parents shed some light on potential public understanding of and perspectives on tDCS and children’s/adolescents’ participation in research in general. Some parents realized after the interview that the complexity and unknowns of the stimulations are greater than they had initially envisaged. Several decided to spend more time exploring tDCS and to inform themselves better. It should be noted, however, that parents still felt sufficiently well informed and did not consider withdrawing their consent for the OptiStim study.
An important finding that emerged from the parent interviews relates to their views on tDCS versus pharmacology. Many parents expressed the view that participation in non-pharmacological studies is safer than, for example, new drug studies. This was also reflected in their consideration of tDCS as a potentially safer treatment for neurological disorders compared with medication. Since the children participating in the study were from a typically developing cohort, the parental views assumption was rooted in a belief that, unlike medication, tDCS has no systemic effects—that is, it affects only the brain and no other organs. Hence, tDCS treatment was perceived as more targeted. In seeing tDCS as something external and more within the user’s control, participants also perceived it as relatively safe. Many of the interviewees did not raise any issues regarding potential side effects (either short- or long-term). This rather optimistic and worry-free approach to tDCS may have been influenced by the terminology used around this technique. Unlike, for example, deep brain stimulation, tDCS is described as non-invasive transcranial brain stimulation, and the ambiguity of this term might lead to confusion or influence risk-benefits assessments of the technique [21, 40]. This is an important finding with an ethical relevance. It shows the grounds for further expansion of misinformation and hype around tDCS and similar techniques and devices [68]. Parents’ short-sightedness in this regard, with a lack of understanding regarding the potential side effects of tDCS, is significant. They focused only on the negative effects of medication, neglecting the actual beneficial effects it can have [69], notwithstanding the fact that tDCS’s efficacy is still being researched and discussed [70]. Thus, parents showed signs of overconfidence in tDCS and simultaneous overestimation of the problematic aspects of medication. It should be noted that although parents regarded tDCS as a better potential therapeutic approach, they had no specific expectations, worries, or wishes about tDCS. However, the lack of expectations and worries may be related to their limited knowledge of tDCS and the fact that most parents had not engaged with this topic prior to the study.
Regarding the use of tDCS for non-medical purposes, most of the parents were against using it in minors, which reflects the current debate on this matter [41]. Similarly, as has already been discussed in the literature, parents observed that enhancement might not be in a child’s best interest [71]. However, in their argumentation, parents focused on safety and the risk of becoming dependent rather than explicitly discussing the importance of protecting their children’s future autonomy or potential threats to the authenticity of a user [66]. The lack of discussion of the potential effects of tDCS and how it might impact the child’s autonomy and future choices was surprising, particularly considering some parents’ remarks that they would like tDCS to improve their children’s abilities.
Another important finding was parents’ lack of knowledge of DIY tDCS application. This may require further attention, as children introduced to the technique during the tDCS study may try to search for it online and experiment with it. It is important to make parents more aware of the DIY possibilities, YouTube videos on subject, and overall ethical issues surrounding direct-to-consumer tDCS applications [72, 73], so that they have the opportunity to address this issue with their children in a timely manner and prevent harmful use.
The interviews also revealed that some parents had little comprehension about tDCS and the overall aims of the study. Despite the efforts to improve the process of provision of informed consent in the clinical studies, this remains a systemic problem [74,75,76]. However, many of the parents expressed strong trust in research and the research team – this was often motivated by previous experiences with research. While trust in research might be considered positive (e.g., many parents knew about ethics approval requirements), this rather relaxed approach to their children’s participation in a clinical study raises concerns and highlights the researchers’ responsibility to ensure that parents do indeed understand and appreciate the risks involved.
The interviews’ narratives show that healthy cohorts might provide important insights into risk-assessment of tDCS. The responses gained in the interviews helped to map the blind spots in parental understanding of how the technique works, what the state of research is, and of current commercial application. This is salient information that would be worth bringing to the process of ethical, responsible translation from research to the clinic.
Limitations of the Study
This study only discussed the views of participants who decided to participate in the tDCS study, which could be a confounder for the general openness and curiosity toward research that emerged from the collected data. Even though special attention was paid to keeping the interview questions open and nonsuggestive, it is possible that the types of the questions asked influenced the direction of the interview. This may also have impacted the positive responses and attitudes toward stimulation. There are very few studies with healthy participants and tDCS and hence there are no reference points that could help improve the study. One way of improving the topic guide in the future would be the inclusion of the member of a public and patient representative in the process of designing the topic guide.
Furthermore, due to the design of the OptiStim, neither the interviewer nor the interviewed minors and their parents in this interview study knew when the minors received actual stimulation (verum) or placebo (sham). It must be also stressed that a qualitative interview study is not representative. More skeptical or critical voices could have emerged from participants recruited in a different setting, different tDCS study or different location. Moreover, the study was conducted in Germany among a relatively small sample, and while the identified problems could be generalizable for most research on tDCS, some issues might be context-specific. Nevertheless, this study may serve as a starting point for further research exploring various stakeholders’ views on tDCS and its ethical and social implications. This is particularly important considering increasing interest in this technique and the scarce research into stakeholders’—participants’ and users’—views in this context. Lastly, we would like to point out the gender imbalance in our sample, both among children and adolescent participant and among parents. We interviewed 11 girls and only 7 boys. The gender imbalance was even more profound in the parents’ sample: out of 18 parents, only 5 fathers participated. There are at least two possibilities for explaining this situation: it could show that women are more curious about the new technologies and/or that women are generally taking over more caring roles, including accompanying children during research participation.
Conclusion
This was the first study to explore the views of typically developing children and adolescents undergoing tDCS and their parents. The participants interviewed are not experts on tDCS and they did not have any particular interest in tDCS as potential treatment for neurological disorder. Their insights were important in capturing their understanding of tDCS and potential misconceptions about the technique. Furthermore, the interviews aimed to explore their views and understanding of cognitive enhancement, including enhancement in children and adolescents. Moreover, tDCS may be introduced in the future as a home therapy, and their views provided hands-on experience that facilitated a discussion around the potential benefits and risks associated with using tDCS at home. To a significant extent, the study reflects the difficulties associated with conducting research among children and adolescents. Despite detailed information, parents exhibited a lack of understanding of the current state of tDCS research (including the discussion around evidence [68, 77]) which may have contributed to the fact some regard brain stimulation as safer than medication, neglecting the role of long-term studies and evidence collected over several years. Rather, negative and poorly informed views on cognitive enhancement highlight the need to strengthen the societal debate on enhancement in which the key pro and con arguments and more nuanced understanding of enhancement are presented and the broader societal impact is discussed. We propose that guidelines for studies of non-invasive transcranial brain stimulation are further developed to include exploration of the ethical issues and current state of research. These should be conducted as a standard in children/adolescents studies and their parents in addition to the questionnaires regarding side effects. Finally, the narratives from the interviews show a specific understanding of safety that was expressed by readiness and interest in participation in the study on brain stimulation. Simultaneously, parents expressed reluctance to signing up their children for pharmacological trials. These issues require further exploration to better understand how potential participants assess risks in tDCS research. This is especially important in paediatric typically developing cohort groups, where the recruitment is particularly challenging due to the vulnerability related to children and adolescents as potential study participants.
Notes
According to clinicaltrials.gov 111 tDCS were registered between 2001–2011 in comparison to 1006 studies in the last ten years (2012–2022), stand April 2022.
The topic guide for children/adolescents did not include any questions about DIY or tDCS devices available online.
The OptiStim study also takes place also at the University of Coimbra in Portugal. Portugal does not allow financial reimbursement for study participants and thus they do not receive any payment for their participation in the study. Participants and their families are reimbursed with costs for traveling, meals, and accommodation through payment of daily allowances.
References
Holdefer, R.N., R. Sadleir, and M.J. Russell. 2006. Predicted current densities in the brain during transcranial electrical stimulation. Clinical Neurophysiology 117 (6): 1388–1397.
Lefaucheur, J.P., A. Antal, S.S. Ayache, D.H. Benninger, J. Brunelin, F. Cogiamanian, et al. 2017. Evidence-based guidelines on the therapeutic use of transcranial direct current stimulation (tDCS). Clinical Neurophysiology 128 (1): 56–92.
Radman, T., A. Datta, R.L. Ramos, J.C. Brumberg, and M. Bikson. 2009. One-dimensional representation of a neuron in a uniform electric field. Annual International Conference of the IEEE Engineering in Medicine and Biology Society 2009: 6481–6484.
Polania, R., M.A. Nitsche, and C.C. Ruff. 2018. Studying and modifying brain function with non-invasive brain stimulation. Nature Neuroscience 21 (2): 174–187.
Ridding, M.C., and U. Ziemann. 2010. Determinants of the induction of cortical plasticity by non-invasive brain stimulation in healthy subjects. The Journal of Physiology. 588 (Pt 13): 2291–2304.
Fitzgerald, P.B., and R.A. Segrave. 2015. Deep brain stimulation in mental health: Review of evidence for clinical efficacy. The Australian and New Zealand journal of psychiatry. 49 (11): 979–993.
Agarwal, S.M., V. Shivakumar, A. Bose, A. Subramaniam, H. Nawani, H. Chhabra, et al. 2013. Transcranial direct current stimulation in schizophrenia. Clin Psychopharmacol Neuroscience 11 (3): 118–125.
Salehinejad, MA, Nejati, V, Mosayebi-Samani, M, Mohammadi, A, Wischnewski, M, Kuo, MF, Avenanti, A, Vicario, CM, Nitsche, MA. 2020 . Transcranial direct current stimulation in adhd: a systematic review of efficacy, safety, and protocol-induced electrical field modeling results. Neuroscience Bulletin 36 (10):1191–1212. https://doi.org/10.1007/s12264-020-00501-x
Jog, M.V., D.J.J. Wang, and K.L. Narr. 2019. A review of transcranial direct current stimulation (tDCS) for the individualized treatment of depressive symptoms. Personalized Medicine in Psychiatry 17–18: 17–22.
Palm, U., A. Hasan, W. Strube, and F. Padberg. 2016. tDCS for the treatment of depression: A comprehensive review. European Archives of Psychiatry and Clinical Neuroscience 266 (8): 681–694.
Fregni, F., M.M. El-Hagrassy, K. Pacheco-Barrios, S. Carvalho, J. Leite, M. Simis, et al. 2020. Evidence-Based Guidelines and Secondary Meta-Analysis for the Use of Transcranial Direct Current Stimulation in Neurological and Psychiatric Disorders. International Journal of Neuropsychopharmacology. 24 (4): 256–313.
Chase, H.W., M.A. Boudewyn, C.S. Carter, and M.L. Phillips. 2020. Transcranial direct current stimulation: A roadmap for research, from mechanism of action to clinical implementation. Molecular Psychiatry 25 (2): 397–407.
Antal, A., I. Alekseichuk, M. Bikson, J. Brockmoller, A.R. Brunoni, R. Chen, et al. 2017. Low intensity transcranial electric stimulation: Safety, ethical, legal regulatory and application guidelines. Clinical Neurophysiology 128 (9): 1774–1809.
Buchanan, DM, Bogdanowicz, T, Khanna N, Lockman-Dufour, G, Robaey, P, D'Angiulli, A. 2021. Systematic review on the safety and tolerability of transcranial direct current stimulation in children and adolescents. Brain Sciences 11 (2):212. https://doi.org/10.3390/brainsci11020212
Rakhade, S.N., and F.E. Jensen. 2009. Epileptogenesis in the immature brain: Emerging mechanisms. Nature Reviews. Neurology 5 (7): 380–391.
Rivera-Urbina, G.N., M.A. Nitsche, C.M. Vicario, and A. Molero-Chamizo. 2017. Applications of transcranial direct current stimulation in children and pediatrics. Reviews in the Neurosciences. 28 (2): 173–184.
Davis, N.J. 2021. Variance in cortical depth across the brain surface: Implications for transcranial stimulation of the brain. European Journal of Neuroscience 53 (4): 996–1007.
Hunold, A., J. Haueisen, C.M. Freitag, M. Siniatchkin, and V. Moliadze. 2021. Cortical current density magnitudes during transcranial direct current stimulation correlate with skull thickness in children, adolescent and young adults. Progress in Brain Research 264: 41–56.
Graham, J., and D. Coghill. 2008. Adverse Effects of Pharmacotherapies for Attention-Deficit Hyperactivity Disorder. CNS Drugs 22 (3): 213–237.
Davis NJ. 2014. Transcranial stimulation of the developing brain: A plea for extreme caution. Frontiers in Human Neuroscience 8(AUG).
Sierawska A, Prehn-Kristensen A, Moliadze V, Krauel K, Nowak R, Freitag CM, et al. 2019. Unmet Needs in Children With Attention Deficit Hyperactivity Disorder-Can Transcranial Direct Current Stimulation Fill the Gap? Promises and Ethical Challenges. Frontiers in Psychiatry 10:334.
Breitling, C., T. Zaehle, M. Dannhauer, J. Tegelbeckers, H.-H. Flechtner, and K. Krauel. 2020. Comparison between conventional and HD-tDCS of the right inferior frontal gyrus in children and adolescents with ADHD. Clinical Neurophysiology. 131 (5): 1146–1154.
Nwaroh, C., A. Giuffre, L. Cole, T. Bell, H.L. Carlson, F.P. MacMaster, et al. 2020. Effects of Transcranial Direct Current Stimulation on GABA and Glx in Children: A pilot study. PLOS ONE 15 (1): e0222620.
Moliadze, V., T. Schmanke, S. Andreas, E. Lyzhko, C.M. Freitag, and M. Siniatchkin. 2015. Stimulation intensities of transcranial direct current stimulation have to be adjusted in children and adolescents. Clinical neurophysiology : Official journal of the International Federation of Clinical Neurophysiology. 126 (7): 1392–1399.
Ciechanski, P., and A. Kirton. 2017. Transcranial Direct-Current Stimulation Can Enhance Motor Learning in Children. Cerebral Cortex 27 (5): 2758–2767.
Singh, I., and K.J. Kelleher. 2010. Neuroenhancement in Young People: Proposal for Research, Policy, and Clinical Management. AJOB Neuroscience. 1 (1): 3–16.
Dubljević, V., V. Saigle, and E. Racine. 2014. The Rising Tide of tDCS in the Media and Academic Literature. Neuron 82 (4): 731–736.
Lucena, M.F.G., P.E.P. Teixeira, C. Bonin Pinto, and F. Fregni. 2019. Top 100 cited noninvasive neuromodulation clinical trials. Expert Review of Medical Devices 16 (6): 451–466.
Nuffield Council on Bioethics. 2015. Children and clinical research: ethical issues. London.
Brett, J., S. Staniszewska, C. Mockford, S. Herron-Marx, J. Hughes, C. Tysall, et al. 2014. A systematic review of the impact of patient and public involvement on service users, researchers and communities. Patient 7 (4): 387–395.
Woolf, S.H. 2008. The Meaning of Translational Research and Why It Matters. JAMA 299 (2): 211–213.
Wexler, A. 2016. The practices of do-it-yourself brain stimulation: Implications for ethical considerations and regulatory proposals. Journal of Medical Ethics. 42 (4): 211–215.
Wexler, A. 2018. Who uses direct-to-consumer brain stimulation products, and why? A study of home users of tDCS devices. J Cogn Enhanc 2, 114–134. https://doi.org/10.1007/s41465-017-0062-z
Fregni, F., M.A. Nitsche, C.K. Loo, A.R. Brunoni, P. Marangolo, J. Leite, et al. 2015. Regulatory Considerations for the Clinical and Research Use of Transcranial Direct Current Stimulation (tDCS): Review and recommendations from an expert panel. Clinical research and regulatory affairs. 32 (1): 22–35.
Maslen H, Douglas T, Cohen Kadosh R, Levy N, Savulescu J. 2015. The regulation of cognitive enhancement devices: refining Maslen et al.'s model. Journal of Law and the Biosciences 2(3):754–67.
Zandvakili, A., Y.A. Berlow, L.L. Carpenter, and N.S. Philip. 2019. Transcranial Direct Current Stimulation in Psychiatry: What Psychiatrists Need to Know. Focus (Am Psychiatr Publ) 17 (1): 44–49.
Thomson H. 2019. Europe’s first home brain-zap device for depression launched in UK. Newscientist. https://www.newscientist.com/article/2221743-europes-first-home-brain-zap-device-for-depression-launched-in-uk/. Accessed 10.03.2022
Nuraleve. 2021. [Available from: https://www.nuraleve.com. Accessed: 10.03.2022
Ritchie, L, Ormston, Nicholls. 2014. Qualitative research practice: Sage.
Davis, NJ, van Koningsbruggen, MG. 2013. "Non-invasive" brain stimulation is not non-invasive. Frontiers in Systems Neuroscience 7:76. https://doi.org/10.3389/fnsys.2013.00076
Maslen, H., B.D. Earp, R. Cohen Kadosh, and J. Savulescu. 2014. Brain stimulation for treatment and enhancement in children: An ethical analysis. Frontiers in Human Neuroscience 8: 953.
Rivera-Urbinaa, G.N., M.A. Nitsche, C.M. Vicario, and A. Molero-Chamizo. 2017. Applications of transcranial direct current stimulation in children and pediatrics. Reviews in the Neurosciences. 28 (2): 173–184.
MacMaster FP, Sembo M, Ma K, Croarkin P. 2016. Brain stimulation in childhood mental health: Therapeutic applications. Pediatric brain stimulation: Mapping and modulating the developing brain. San Diego, CA: Elsevier Academic Press; US; p. 321–44.
Muszkat, D., G.V. Polanczyk, T.G.C. Dias, and A.R. Brunoni. 2016. Transcranial Direct Current Stimulation in Child and Adolescent Psychiatry. Journal of Child and Adolescent Psychopharmacology. 26 (7): 590–597.
Wurzman, R.P., and R.H. Hamilton. 2016. Ethical Aspects of tDCS Use in Neuropsychiatry and the Risk of Misuse. In Transcranial Direct Current Stimulation in Neuropsychiatric Disorders: Clinical Principles and Management, ed. A. Brunoni, M. Nitsche, and C. Loo, 363–382. Cham: Springer International Publishing.
Palm, U., F.M. Segmiller, A.N. Epple, F.J. Freisleder, N. Koutsouleris, G. Schulte-Korne, et al. 2016. Transcranial direct current stimulation in children and adolescents: A comprehensive review. Journal of Neural Transmission (Vienna) 123 (10): 1219–1234.
Cohen Kadosh, R., N. Levy, J. O’Shea, N. Shea, and J. Savulescu. 2012. The neuroethics of non-invasive brain stimulation. Current Biology : CB. 22 (4): R108–R111.
Poleszczyk A, Antosik-Wojcinska AZ. 2015. Transcranial direct current stimulation-possible therapeutic applications in psychiatric disorders in adults and children. [Polish]. Family Medicine and Primary Care Review. 17(4):341–6.
Rubio-Morell, B., A. Rotenberg, S. Hernandez-Exposito, and A. Pascual-Leone. 2011. The use of noninvasive brain stimulation in childhood psychiatric disorders: New diagnostic and therapeutic opportunities and challenges. Revista de Neurologia. 53 (4): 209–225.
Kail RV. 2011. Children and Their Development. 6th ed. N.J: Prentice Hall.: Englewood Cliffs.
Gandiga, P.C., F.C. Hummel, and L.G. Cohen. 2006. Transcranial DC stimulation (tDCS): A tool for double-blind sham-controlled clinical studies in brain stimulation. Clinical Neurophysiology 117 (4): 845–850.
Low, J. 2019. A Pragmatic Definition of the Concept of Theoretical Saturation. Sociological Focus. 52 (2): 131–139.
Antal, A., D. Terney, C. Poreisz, and W. Paulus. 2007. Towards unravelling task-related modulations of neuroplastic changes induced in the human motor cortex. The European Journal of Neuroscience. 26 (9): 2687–2691.
Braun, V., and V. Clarke. 2006. Using thematic analysis in psychology. Qualitative Research in Psychology. 3 (2): 77–101.
VERBI S. 2018. MAXQDA. Berlin Germany.
Saunders, B., J. Sim, T. Kingstone, S. Baker, J. Waterfield, B. Bartlam, et al. 2018. Saturation in qualitative research: Exploring its conceptualization and operationalization. Quality & Quantity. 52 (4): 1893–1907.
Palm U, Kumpf U, Behler N, Wulf L, Kirsch B, Wörsching J, et al. 2018. Home Use, Remotely Supervised, and Remotely Controlled Transcranial Direct Current Stimulation: A Systematic Review of the Available Evidence. Neuromodulation: Technology at the Neural Interface. 21(4):323–33
Splittgerber, M, Japaridze, N, Sierawska, A, Gimenez, S, Nowak, R, Siniatchkin, M, Moliadze, V. 2020. First generalized tonic clonic seizure in the context of pediatric tDCS - A case report. Neurophysiologie Clinique 50 (1): 69–72. https://doi.org/10.1016/j.neucli.2019.11.002
Sierawska, A., V. Moliadze, M. Splittgerber, A. Rogge, M. Siniatchkin, and A. Buyx. 2020. First Epileptic Seizure and Initial Diagnosis of Juvenile Myoclonus Epilepsy (JME) in a Transcranial Direct Current Stimulation (tDCS) Study– Ethical Analysis of a Clinical case. Neuroethics 13 (3): 347–351.
Buchanan, DM, D'Angiulli, A, Samson, A, Maisonneuve, AR, Robaey, P. 2022. Acceptability of transcranial direct current stimulation in children and adolescents with ADHD: The point of view of parents. Journal of Health Psychology 27 (1): 36–46. https://doi.org/10.1177/1359105320937059
Sierawska, A., A. Prehn-Kristensen, H. Brauer, K. Krauel, C. Breitling-Ziegler, M. Siniatchkin, et al. 2021. Transcranial direct-current stimulation and pediatric attention deficit hyperactivity disorder (ADHD)-Findings from an interview ethics study with children, adolescents, and their parents. Progress in Brain Research 264: 363–386.
Stunkel, L., and C. Grady. 2011. More than the money: A review of the literature examining healthy volunteer motivations. Contemporary Clinical Trials 32 (3): 342–352.
Rice, M., and M.E. Broome. 2004. Incentives for Children in Research. Journal of Nursing Scholarship. 36 (2): 167–172.
Broome ME, Kodish E, Geller G, Siminoff LA. 2003 Children in research: new perspectives and practices for informed consent. Irb Suppl 25(5):S20-s3
Sabini, J., and J. Monterosso. 2005. Judgments of the fairness of using performance enhancing drugs. Ethics and Behavior 15 (1): 81–94.
Schuijer, J.W., I.M. de Jong, F. Kupper, and N.M. van Atteveldt. 2017. Transcranial Electrical Stimulation to Enhance Cognitive Performance of Healthy Minors: A Complex Governance Challenge. Frontiers in Human Neuroscience 11: 142.
Lavazza, A. 2017. Can Neuromodulation also Enhance Social Inequality? Some Possible Indirect Interventions of the State. Frontiers in Human Neuroscience 11: 113.
Horvath JC. 2019. 18 - Noninvasive brain stimulation: When the hype transcends the evidence. In: Raz A, Thibault RT, editors. Casting Light on the Dark Side of Brain Imaging: Academic Press. p. 107–11.
Vaughan, B.S., J.S. March, and C.J. Kratochvil. 2012. The evidence-based pharmacological treatment of paediatric ADHD. International Journal of Neuropsychopharmacology. 15 (1): 27–39.
Kekic, M., E. Boysen, I.C. Campbell, and U. Schmidt. 2016. A systematic review of the clinical efficacy of transcranial direct current stimulation (tDCS) in psychiatric disorders. Journal of Psychiatric Research. 74: 70–86.
Wagner, K., H. Maslen, J. Oakley, and J. Savulescu. 2018. Would you be willing to zap your child’s brain? Public perspectives on parental responsibilities and the ethics of enhancing children with transcranial direct current stimulation. AJOB Empirical Bioethics 9 (1): 29–38.
Wurzman, R., R.H. Hamilton, A. Pascual-Leone, and M.D. Fox. 2016. An open letter concerning do-it-yourself users of transcranial direct current stimulation. Annals of Neurology. 80 (1): 1–4.
Wexler, A. 2017. The social context of "do-it-yourself" brain stimulation: Neurohackers, Biohackers, and Lifehackers. Frontiers in Human Neuroscience 11:224. https://doi.org/10.3389/fnhum.2017.00224
Hereu, P., E. Pérez, I. Fuentes, X. Vidal, P. Suñé, and J.M. Arnau. 2010. Consent in clinical trials: What do patients know? Contemporary Clinical Trials 31 (5): 443–446.
Sherlock, A., and S. Brownie. 2014. Patients’ recollection and understanding of informed consent: A literature review. ANZ Journal of Surgery 84 (4): 207–210.
Tam, N.T., N.T. Huy, T.B. le Thoa, N.P. Long, N.T. Trang, K. Hirayama, et al. 2015. Participants’ understanding of informed consent in clinical trials over three decades: Systematic review and meta-analysis. Bulletin of the World Health Organization 93 (3): 186–198.
Horvath, J.C., J.D. Forte, and O. Carter. 2015. Evidence that transcranial direct current stimulation (tDCS) generates little-to-no reliable neurophysiologic effect beyond MEP amplitude modulation in healthy human subjects: A systematic review. Neuropsychologia 66: 213–236.
Acknowledgements
We would like to thank the OptiStim study participants and their parents for their time and contribution to the study.
Funding
Open Access funding enabled and organized by Projekt DEAL. This project has received funding from the European Union’s Horizon 2020 research and innovation program under grant agreement no. 731827. This text reflects only the authors’ views and the Commission is not liable for any use that may be made of the information contained therein.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interest
All authors declare no competing interests.
Ethics Approval
Approval was obtained from the local ethics committee: Ethics Committee University Medical Center Schleswig–Holstein, approval number D 449/17.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sierawska, A., Splittgerber, M., Moliadze, V. et al. Transcranial Direct Current Stimulation (tDCS) in Pediatric Populations—– Voices from Typically Developing Children and Adolescents and their Parents. Neuroethics 16, 3 (2023). https://doi.org/10.1007/s12152-022-09507-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12152-022-09507-w