Abstract
Background
Electroencephalography (EEG) neurofeedback is a type of biofeedback that purportedly teaches users how to control their brainwaves. Although neurofeedback is currently offered by thousands of providers worldwide, its provision is contested, as its effectiveness beyond a placebo effect is unproven. While scholars have voiced numerous ethical concerns about neurofeedback—regarding opportunity cost, physical and psychological harms, financial cost, and informed consent—to date these concerns have remained theoretical. This pilot study aimed to provide insights on whether these issues were supported by empirical data from the experiences of neurofeedback users.
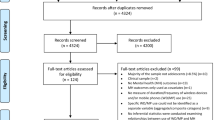
Methods
Semi-structured telephone interviews were conducted with individuals who had used EEG neurofeedback for themselves and/or for a child.
Results
The majority of respondents (N = 36) were female (75%), white (92%), and of higher socioeconomic status relative to the U.S. population. Among adult users (n = 33), most (78.8%) resorted to neurofeedback after having tried other therapies, and were satisfied with the treatment (81.8%). The majority paid for neurofeedback out-of-pocket (72.7%) and considered it to be good value for money (84.8%). More than half (57.6%) considered neurofeedback to be a scientifically well-established therapy. However, of those, 78.9% were using neurofeedback for indications not adequately supported by scientific evidence.
Conclusion
Concerns regarding opportunity cost, physical and psychological harms, and financial cost are not substantiated by our findings. Our results partially support concerns regarding insufficient understanding of limitations. This study underlines the disconnect between some of the theoretical concerns raised by scholars regarding the use of non-validated therapies and the lived experiences of users.
Similar content being viewed by others
References
Marzbani, Hengameh, HamidReza Marateb, and Marjan Mansourian. 2016. Neurofeedback: A comprehensive review on system design, methodology and clinical applications. Basic and Clinical Neuroscience 7: 143–158. https://doi.org/10.15412/j.bcn.03070208.
Kamiya, Joe. 1968. Conscious Control of Brain Waves. Psychology Today.
Ossadtchi, Alexei, Tatiana Shamaeva, Elizaveta Okorokova, Victoria Moiseeva, and Mikhail A. Lebedev. 2017. Neurofeedback learning modifies the incidence rate of alpha spindles, but not their duration and amplitude. Scientific Reports 7: 3772. https://doi.org/10.1038/s41598-017-04012-0.
Wexler, Anna, Ashwini Nagappan, Deena Kopyto, and Rebekah Choi. 2020. Neuroenhancement for sale: Assessing the website claims of neurofeedback providers in the USA. Journal of Cognitive Enhancement: 1–10. https://doi.org/10.1007/s41465-020-00170-8.
Thibault, Robert T., and Amir Raz. 2017. The psychology of neurofeedback: Clinical intervention even if applied placebo. American Psychologist 72: 679–688. https://doi.org/10.1037/amp0000118.
Kohl, Simon H., David M. A. Mehler, Michael Lührs, Robert T. Thibault, Kerstin Konrad, and Bettina Sorger. 2020. The potential of functional near-infrared spectroscopy-based neurofeedback—a systematic review and recommendations for best practice. Frontiers in Neuroscience 14: 594. https://doi.org/10.3389/fnins.2020.00594.
Thibault, Robert T., Amanda MacPherson, Michael Lifshitz, Raquel R. Roth, and Amir Raz. 2018. Neurofeedback with fMRI: A critical systematic review. NeuroImage 172: 786–807. https://doi.org/10.1016/j.neuroimage.2017.12.071.
Tursic, Anita, Judith Eck, Michael Lührs, David E. J. Linden, and Rainer Goebel. 2020. A systematic review of fMRI neurofeedback reporting and effects in clinical populations. NeuroImage: Clinical 28: 102496. https://doi.org/10.1016/j.nicl.2020.102496.
International Society for Neuroregulation and Research (ISNR). 2017. In Defense of Neurofeedback. https://isnr.org/in-defense-of-neurofeedback Accessed 18 Sep 2022.
Wexler, Anna, and Robert Thibault. 2018. Mind-reading or misleading? Assessing direct-to-consumer electroencephalography (EEG) devices marketed for wellness and their ethical and regulatory implications. Journal of Cognitive Enhancement 3: 131–137. https://doi.org/10.1007/s41465-018-0091-2.
Kalokairinou, Louiza, Laura Specker Sullivan, and Anna Wexler. 2021. Neurofeedback as placebo: a case of unintentional deception? Journal of Medical Ethics: medethics-2021–107435. https://doi.org/10.1136/medethics-2021-107435.
Purper-Ouakil, Diane, Hilario Blasco-Fontecilla, Tomas Ros, Eric Acquaviva, Tobias Banaschewski, Sarah Baumeister, Elisa Bousquet, et al. 2022. Personalized at-home neurofeedback compared to long-acting methylphenidate in children with ADHD: NEWROFEED, a European randomized noninferiority trial. Journal of Child Psychology and Psychiatry 63: 187–198. https://doi.org/10.1111/jcpp.13462.
Louthrenoo, Orawan, Nonglak Boonchooduang, Narueporn Likhitweerawong, Kittipat Charoenkwan, and Manit Srisurapanont. 2021. The effects of neurofeedback on executive functioning in children with ADHD: A meta-analysis. Journal of Attention Disorders: 108705472110457. https://doi.org/10.1177/10870547211045738.
Gandara, Veronica, Jaime A. Pineda, I-Wei. Shu, and Fiza Singh. 2020. A Systematic review of the potential use of neurofeedback in patients with Schizophrenia. Schizophrenia Bulletin Open 1: sgaa005. https://doi.org/10.1093/schizbullopen/sgaa005.
Arns, Martijn, C. Richard Clark, Mark Trullinger, and Roger deBeus, Martha Mack, and Michelle Aniftos. 2020. Neurofeedback and Attention-Deficit/Hyperactivity-Disorder (ADHD) in children: Rating the evidence and proposed guidelines. Applied Psychophysiology and Biofeedback 45: 39–48. https://doi.org/10.1007/s10484-020-09455-2.
Duric, Nezla S., Jørg. Assmus, Doris Gundersen, and Irene B. Elgen. 2012. Neurofeedback for the treatment of children and adolescents with ADHD: A randomized and controlled clinical trial using parental reports. BMC Psychiatry 12: 107. https://doi.org/10.1186/1471-244x-12-107.
Arnold, L Eugene, Nicholas Lofthouse, Sarah Hersch, Xueliang Pan, Elizabeth Hurt, Bethany Bates, Kathleen Kassouf, Stacey Moone, and Cara Grantier. 2012. EEG neurofeedback for ADHD: Double-blind sham-controlled randomized pilot feasibility trial. Journal of Attention Disorders 17: 410–419. https://doi.org/10.1177/1087054712446173.
Trambaiolli, Lucas R., Simon H. Kohl, David E.J.. Linden, and David M.A.. Mehler. 2021. Neurofeedback training in major depressive disorder: A systematic review of clinical efficacy, study quality and reporting practices. Neuroscience & Biobehavioral Reviews 125: 33–56. https://doi.org/10.1016/j.neubiorev.2021.02.015.
Thibault, Robert T., Michael Lifshitz, and Amir Raz. 2017. Neurofeedback or neuroplacebo? Brain 140: 862–864. https://doi.org/10.1093/brain/awx033.
The Neurofeedback Collaborative Group, L. Eugene Arnold, Martijn Arns, Justin Barterian, Rachel Bergman, C. Sarah Black, Keith Conners, et al. 2020. Double-blind placebo-controlled randomized clinical trial of neurofeedback for Attention-Deficit/Hyperactivity disorder with 13-Month Follow-up. Journal of the American Academy of Child & Adolescent Psychiatry. https://doi.org/10.1016/j.jaac.2020.07.906.
Thibault, Robert T., Samuel Veissière, Jay A. Olson, and Amir Raz. 2018. Treating ADHD with suggestion: Neurofeedback and placebo therapeutics. Journal of Attention Disorders 22: 707–711. https://doi.org/10.1177/1087054718770012.
Nagappan, Ashwini, Louiza Kalokairinou, and Anna Wexler. 2021. Ethical and Legal Considerations of Alternative Neurotherapies. AJOB Neuroscience: 1–13. https://doi.org/10.1080/21507740.2021.1896601.
Boser, Urlich. 2017. Betsy DeVos has invested millions in this ‘brain training’ company. So I checked it out.
Hammond, Corydon, and Lynda Kirk. 2007. Negative effects and the need for standards of practice in neurofeedback. Biofeedback 35: 139–145.
Ellison, Katherine. 2010. Neurofeedback Gains Popularity and Lab Attention.
Thibault, Robert T., Michael Lifshitz, Niels Birbaumer, and Amir Raz. 2015. Neurofeedback, self-regulation, and brain imaging: Clinical science and fad in the service of mental disorders. Psychotherapy and Psychosomatics 84: 193–207. https://doi.org/10.1159/000371714.
Wexler, Anna, Ashwini Nagappan, Deena Kopyto, and Rebekah Choi. 2020. Neuroenhancement for sale: Assessing the website claims of neurofeedback providers in the USA. Journal of Cognitive Enhancement 4: 379–388. https://doi.org/10.1007/s41465-020-00170-8.
Pray, W Steven. 2006. Ethical, scientific, and educational concerns with unproven medications. American Journal of Pharmaceutical Education 70: 141. https://doi.org/10.5688/aj7006141.
Mastroleo, Ignacio, and Felicitas Holzer. 2020. New non-validated practice: An enhanced definition of innovative practice for medicine. Law, Innovation and Technology 12: 1–29. https://doi.org/10.1080/17579961.2020.1815405.
Mastroleo, Ignacio, and Timothy Daly. 2021. Seeing the forest for the trees: The importance of unifying ethical and legal considerations for non-validated practice of neurotherapies. AJOB Neuroscience 12: 270–272. https://doi.org/10.1080/21507740.2021.1973149.
Anderson, James A., Ania Mizgalewicz, and Judy Illes. 2013. Triangulating perspectives on functional neuroimaging for disorders of mental health. BMC Psychiatry 13: 208. https://doi.org/10.1186/1471-244x-13-208.
Stone, J. 2000. Ethical issues in complementary and alternative medicine. Complementary Therapies in Medicine 8: 207–213. https://doi.org/10.1054/ctim.2000.0385.
Ernst, Edzard, Michael H. Cohen, and James L. Stone. 2004. Ethical problems arising in evidence based complementary and alternative medicine. Journal of Medical Ethics 30: 156–159. https://doi.org/10.1136/jme.2003.007021.
Shaw, David M. 2010. Homeopathy is where the harm is: Five unethical effects of funding unscientific ‘remedies.’ Journal of Medical Ethics 36: 130. https://doi.org/10.1136/jme.2009.034959.
Clark, Peter A. 2000. The ethics of alternative medicine therapies. Journal of Public Health Policy 21: 447–470. https://doi.org/10.2307/3343283.
Monaco, Grace Powers, and Gilbert Smith. 2002. Informed consent in complementary and alternative medicine: Current status and future needs. Seminars in Oncology 29: 601–608. https://doi.org/10.1053/sonc.2002.50010.
Vohra, Sunita, and Michael H. Cohen. 2007. Ethics of complementary and alternative medicine use in children. Pediatric Clinics of North America 54: 875–884. https://doi.org/10.1016/j.pcl.2007.10.004.
Marcer, H. 2010. Ethical considerations in the use of complementary and alternative medicine for children with autism. Archives of Disease in Childhood 95: A80.2-A80. https://doi.org/10.1136/adc.2010.186338.178.
Gilmour, Joan, Christine Harrison, Michael H. Cohen, and Sunita Vohra. 2011. Pediatric use of complementary and alternative medicine: Legal, ethical, and clinical issues in decision-making. Pediatrics 128: S149–S154. https://doi.org/10.1542/peds.2010-2720b.
Cortese, Samuele, Maite Ferrin, Daniel Brandeis, Martin Holtmann, Pascal Aggensteiner, David Daley, Paramala Santosh, et al. 2016. Neurofeedback for Attention-Deficit/Hyperactivity disorder: Meta-analysis of clinical and neuropsychological outcomes from randomized controlled trials. Journal of the American Academy of Child & Adolescent Psychiatry 55: 444–455. https://doi.org/10.1016/j.jaac.2016.03.007.
Logemann, H.N., Marieke M. Alexander, Titus W D P. Lansbergen, Van Os, Koen B E. Böcker, and JLeon Kenemans. 2010. The effectiveness of EEG-feedback on attention, impulsivity and EEG: A sham feedback controlled study. Neuroscience Letters 479: 49–53. https://doi.org/10.1016/j.neulet.2010.05.026.
U.S. Census Bureau U HINC-01. 2019. Selected Characteristics of Households by Total Money Income.
U. S. Department of Housing and Urban Development. 2021. Estimated Median Family Incomes for Fiscal Year (FY) 2021.
Astin, John A. 1998. Why patients use alternative medicine. JAMA 279: 1548. https://doi.org/10.1001/jama.279.19.1548.
Su, Dejun, and Lifeng Li. 2011. Trends in the use of complementary and alternative medicine in the United States: 2002–2007. Journal of Health Care for the Poor and Underserved 22: 296–310.
Clarke, Tainya C., Patricia M. Barnes, Lindsey I. Black, Barbara J. Stussman, and Richard L. Nahin. 2018. Use of yoga, meditation, and chiropractors among U.S. adults aged 18 and over. NCHS Data Brief.
Bishop, Felicity L., and G.T. Lewith. 2010. Who uses CAM? A narrative review of demographic characteristics and health factors associated with CAM use. Evidence-based Complementary and Alternative Medicine : ECAM 7: 11–28. https://doi.org/10.1093/ecam/nen023.
Zhang, Yan, Lixing Lao, Haiyan Chen, and Rodrigo Ceballos. 2012. Acupuncture use among american adults: What acupuncture practitioners can learn from national health interview survey 2007? Evidence-based Complementary and Alternative Medicine: ECAM 2012: 710750. https://doi.org/10.1155/2012/710750.
Whedon, James M., and Yunjie Song. 2012. Racial Disparities in the Use of Chiropractic Care Under Medicare. Alternative Therapies in Health Medicine 6:20.
Sointu, Eeva. 2021. The Wiley Blackwell Companion to Medical Sociology: 516–536. https://doi.org/10.1002/9781119633808.ch25.
Connor, Linda H. 2004. Relief, risk and renewal: Mixed therapy regimens in an Australian suburb. Social Science & Medicine 59: 1695–1705. https://doi.org/10.1016/j.socscimed.2004.01.030.
Funk, Cary, Brian Kennedy, and Meg Hefferon. 2017. Vast majority of Americans say benefits of childhood vaccines outweigh risks. Pew Research Center.
Cartwright, Tina, and Rebecca Torr. 2005. Making sense of illness: The experiences of users of complementary medicine. Journal of Health Psychology 10: 559–572. https://doi.org/10.1177/1359105305053425.
Sirois, Fuschia M., and Mary L. Gick. 2002. An investigation of the health beliefs and motivations of complementary medicine clients. Social Science & Medicine 55: 1025–1037. https://doi.org/10.1016/s0277-9536(01)00229-5.
Miller, Franklin G., Ezekiel J. Emanuel, Donald L. Rosenstein, and Stephen E. Straus. 2004. Ethical issues concerning research in complementary and alternative medicine. JAMA 291: 599–604. https://doi.org/10.1001/jama.291.5.599.
Garland, Sheila N., David Valentine, Krupali Desai, Susan Li, Corey Langer, Tracey Evans, and Jun J. Mao. 2013. Complementary and alternative medicine use and benefit finding among cancer patients. The Journal of Alternative and Complementary Medicine 19: 876–881. https://doi.org/10.1089/acm.2012.0964.
Wexler, Anna, Rebekah J Choi, Ashwin G Ramayya, Nikhil Sharma, Brendan J McShane, Love Y Buch, Melanie P Donley-Fletcher, et al. 2021. Ethical issues in intraoperative neuroscience research: Assessing subjects’ recall of informed consent and motivations for participation. AJOB Empirical Bioethics: 1–10. https://doi.org/10.1080/23294515.2021.1941415
Falagas, Matthew E., Ioanna P. Korbila, Konstantina P. Giannopoulou, Barbara K. Kondilis, and George Peppas. 2009. Informed consent: How much and what do patients understand? The American Journal of Surgery 198: 420–435. https://doi.org/10.1016/j.amjsurg.2009.02.010.
Verheggen, Frank W.S.M.., and Frans C.B.. van Wijmen. 1996. Informed consent in clinical trials. Health Policy 36: 131–153. https://doi.org/10.1016/0168-8510(95)00805-5.
Sahin, Namık, Alpaslan Oztürk, Yüksel. Ozkan, and Ayşegül Demirhan. Erdemir. 2010. What do patients recall from informed consent given before orthopedic surgery? Acta Orthopaedica et Traumatologica Turcica 44: 469–475. https://doi.org/10.3944/aott.2010.2396.
Fortun, P., J. West, L. Chalkley, A. Shonde, and C. Hawkey. 2008. Recall of informed consent information by healthy volunteers in clinical trials. QJM: An International Journal of Medicine 101 (625): 629. https://doi.org/10.1093/qjmed/hcn067.
Acknowledgements
We would like to thank all participants in our study and the moderators of the Facebook groups who agreed to give us access.
Funding
This study was supported by the Office of the Director, National Institutes of Health (NIH), under Award Number DP5OD026420.
Author information
Authors and Affiliations
Contributions
The study was conceptualized by LK and designed by LK, AN and AW. The interviews were conducted by LK and the data analysis was performed by LK and RC. LK wrote the first draft and all authors revised and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
This study was carried out in accordance with all relevant ethical and legal standards, including the Declaration of Helsinki. The University of Pennsylvania Institutional Review Board reviewed the protocol of this study in July 2020 and determined that the proposal meets eligibility criteria for IRB review exemption (IRB Protocol: #843651). All participants received an informed consent form via email prior to the interview, which was reviewed verbally before commencing each interview.
Competing Interests
The authors have no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kalokairinou, L., Choi, R., Nagappan, A. et al. Opportunity Cost or Opportunity Lost: An Empirical Assessment of Ethical Concerns and Attitudes of EEG Neurofeedback Users. Neuroethics 15, 28 (2022). https://doi.org/10.1007/s12152-022-09506-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12152-022-09506-x