Abstract
The concept of moralisation of health behaviours was introduced in social psychology to describe the attribution of moral properties to habits and conditions like smoking or being a vegetarian. Moral properties are powerful motivators for people and institutions, as they may trigger blame, stigma, and appraisal, as well as the polarisation of interest and scientific hype. Here I extend the concept and illustrate how medicines and treatments can be seen as if they had moral properties, too, when they come to be regarded as good or bad in the moral sense, and not just in the instrumental sense of benefiting or harming health. I propose the hydroxychloroquine (HCQ) controversy of 2020 as an example of moralisation of a medicine. HCQ and chloroquine are anti-malarial drugs, whose off-label use for Covid-19 was hotly discussed in the early months of the pandemic, both in the media and within the scientific community, and eventually dismissed when robust evidence came out. The point of the paper is to show that moralisation of health products and treatments may influence individual and institutional decisions in significant ways, and also affect research. For these reasons, it should be carefully monitored and critically assessed.
Similar content being viewed by others
1 Introduction
Health matters to us, it has value. We judge it as good to have and we may see it as part of our life goals. Derivatively, health-related behaviours such as exercising or smoking have value – they are good and bad for us, respectively, in that they make us healthier or less healthy. In addition to this quite uncontroversial attribution of value to health and health-related behaviours, there is a different attribution; that is, moralisation. To moralise is to judge something as morally good or bad (and not instrumentally or practically good or bad). The concept of moralisation of health behaviours was introduced in social psychology to describe the attribution of moral properties to habits and conditions like smoking or being a vegetarian. Psychologist Paul Rozin (1999) explained that moral properties are powerful motivators for people and institutions, as they may trigger blame, stigma, and appraisal, polarisation of interest and scientific hype, and even a biased appraisal of evidence. The concept has a wide application. Recent studies have shown that any product can be moralised, from fridges to biscuits (Thomas, 2019).
If you can moralise a refrigerator, then you can also moralise a medicine or medical intervention. This article develops this idea, with the aim of adding to the picture of how values enter, positively or negatively, into medical research and practice. To illustrate what moralisation of a medicine can be, I take the HCQ controversy of 2020 as a case study. HCQ and chloroquine are anti-malarial drugs, whose off-label use for Covid-19 was hotly discussed in the early months of the pandemic, both in the media and within the scientific community, and eventually dismissed when robust evidence came out. HCQ was strenuously promoted by US President Donald Trump, among others, and vehemently opposed by supporters of evidence-based medicine; it polarised public opinion and engendered a complex case of publication retraction of a study published in the journal The Lancet (Mehra et al., 2020). I will argue that the concept of moralisation applies to this story and suggest that it may help explain some of its features. Moral properties are very powerful motivators both in personal and in institutional decision settings—an aspect quite evident in the HCQ case. In this sense, moralisation of medicine may interfere with the normal route to the verdict that a medicine is good.
Drawing from psychological research, I will also point out that there are two broad mechanisms of moralisation, one affective-associative, and the other inferential. Distinguishing these may be relevant when the task is to assess or prevent cases of moralisation. This brings me to the more general goal of this article, which is to show that moralisation is relevant for philosophers of medicine interested in how values enter medical research and healthcare. Philosophers of science and bioethicists should individuate and assess cases of moralisation of medicines, interventions, and behaviours by institutions, researchers, patients, medical experts, and professionals. Moralisation may be key to understanding why people follow or do not follow doctors’ prescriptions and the recommendations of healthcare authorities regarding, for example, vaccination or personal preventive measures, such as mask-wearing. It may also bring some light to a reconstruction of what makes a medical intervention controversial, under-researched or over-researched. Think of psychedelic drugs for psychiatric use, for example (Beswerchij & Sisti, 2022; Schwarz-Plaschg, 2022), and again, of mask-wearing during the pandemic (Howard, 2022; Jefferson et al., 2023).
As said, what follows is intended as a contribution to the study of values in medical research and practice. That all scientific research is influenced by values, preferences, and generally by non-epistemic reasons, and that this is an intrinsic feature of science rather than a defect, are widespread convictions among philosophers of science today. Values have a role when scientists choose a research topic, select the goal of their research (i.e., explaining versus policy advising), assess inductive risks (i.e., decide when an experiment or inquiry is complete), decide among competing hypotheses that are equally supported by evidence, and frame and communicate study results (Douglas, 2009; Elliott & McKaughan, 2014; Steel & Whyte, 2012). On a different level, medicine and its specialties are complex social activities in which social norms and social effects related to power, reputation, and gender are in place—for example, in how consensus is reached among experts (Solomon, 2015). Also, the values of researchers and industrial partners in medical research can act as biases (Bueter, 2022; Bueter & Jukola, 2020; Stegenga, 2018). Covid science arguably provided an excellent case study in all these respects. Philosophers have pointed out that Covid science, and evidence-based policies, involved values at many levels, which were rarely if ever recognised and justified by scientists, politicians, and institutions (Amoretti & Lalumera, 2021; Fuller, 2021; Mercuri n.d.). My discussion of moralisation as a case of value-intrusion (possibly with a negative connotation) is meant to add a thread to this already rich “tapestry of values” (Elliott, 2017).
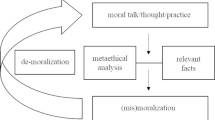
This article is organised into sections. Section 2 surveys the literature on moralisation from its origins with Rozin’s work to more recent developments while emphasising a distinction between processes of moralisation, which are grounded in drawing logical connections between a particular behaviour and accepted moral principles (so-called “rational” processes) on the one hand, and processes grounded in drawing associative-affective connections (or “irrational” processes) on the other. Having established this framework, I will then examine HCQ’s controversial uptake in the effort to fight Covid-19 (Section 3) and show how moralisation was at work on both sides of the HCQ debate, albeit in differing ways (Section 4). In Section 5, I will attempt to show the influence of the moralisation of HCQ on medical research (in the Spring of 2020) by suggesting that it has generated an intrusion of values on two levels: that of the choice of research question and that of the evaluation of evidence, or inductive risk. Section 6 contains my concluding remarks and suggestions on how to study moralisation in healthcare and medical research.
2 Moralization
I prefer coffee over tea, but this does not imply that, for me, tea is morally bad or people who prefer tea are, and I do not think of myself as being a better person because I prefer coffee. If tea and coffee consumption were moralised, such implications would be conceptually allowed. Social psychologist Paul Rozin (1999) defined moralisation as “the process through which preferences are converted into values, both in individual lives and at the level of culture” (p. 218). In his research, Rozin focused on health-related behaviours, such as smoking, and described the moralisation process that occurred in the US (and in most Western countries) in the second half of the twentieth century. Smoking acquired the moral property of being morally bad in itself—not just instrumentally bad because it puts one at risk for health problems—in a period of three generations. Other examples he considered are meat-eating and alcohol and drug (such as opioids) consumption. Meat-eating steadily shifted from a preference to morally bad behaviour with time, while the attribution of moral properties to drug and alcohol consumption tends to vary with time and place (Feinberg et al., 2019; Rozin & Singh, 1999; Rozin et al., 1997).
Though the specific processes of moralisation are historically and culturally specific, what all the considered examples have in common is that they are all behaviours that matter to individual and, arguably, to public health, and that they acquire moral properties by such a link. In a recent article starting from Rozin’s account of moralisation, S. Joshua Thomas (2019) added pediatric vaccination and Covid-19 vaccination in rich Western countries to the list. Let us consider this example in more detail. Those in favour of vaccination may tend to judge it to be not only beneficial to one’s health, but also morally good, for reasons that include protection of the weakest, solidarity, and contribution to health as a common good. They may also tend to believe that not being vaccinated is harmful to others and that harming others is morally bad. This attitude has produced episodes of public blame for anti-vaxxers, and arguments defending their accountability for medical expenses. On the other hand, anti-vaxxers tend to connect vaccination with the greed of Big Pharma, political threats to personal liberty and autonomy, and with violation of one’s body purity and sacredness. As greed, constriction of liberty, and violation of purity are morally bad, those who support and promote vaccination, and even those who just accept it, may inherit the property of moral badness, according to anti-vaxxers.
It is crucial at this point to say why moralisation matters and Rozin’s research was seminal in addressing this point. On the individual level, what is morally laden becomes internalised; that is, it is included in a person’s representation of themself. So, for example, being a non-smoker, or an anti-vaxxer, may become central to who you are, and therefore important to preserve, defend, and justify much more than a mere preference. Consequently, moralised behaviours are reinforced through generations (i.e., transmitted to children or pupils by the ones who have internalised them). Moralisation also promotes overjustification, for example moral vegetarians, compared to health vegetarians, tend to discover and present more non-moral reasons against eating meat. Moralisation of behaviours makes people feel entitled to attitudes of blame and stigma, or pride and admiration. It reinforces in-group cohesion and outgroup exclusion. With moralisation, new virtues and vices are born, such as being a non-smoker, a vegetarian, or an anti-vaxxer if you have certain background beliefs about purity or liberty. Accordingly, social norms promoting such virtues are shaped and enforced (Brandt et al., 2016).
On the institutional level, the effects of moralisation are equally powerful. When a behaviour becomes moralised, governments and other institutions act with the prevention, education, or prohibition, more than they would have done were the behaviour just unhealthy. Moreover, research is mobilised for finding evidence that confirms the goodness or badness of the moralised entity in terms of risk or gain for health. It therefore happens that research funding is catalysed by morally hot topics and diverted from others. For example, on the assumption that divorce is morally bad, psychological research was catalysed on testing the hypothesis that divorce is harmful to children (Anderson, 2004). Moralisation thus affects the structure of knowledge acquisition at many points.
This powerful effect of motivation that moral properties have can be seen as the psychological counterpart of a widely held philosophical thesis, the overridingness of moral properties. Overridingness means prevalence over other evaluative properties in cases of conflict. Faced with a choice, one should opt for what is morally good over what is legal, convenient, or advantageous relative to one’s goals. This does not mean that we always opt for the morally good choice, of course, but that upon reflection, we judge that we should. The moral ought is the primary ought, so to speak (Foot, 1983).
At this point a philosophical question arises: is moralisation justifiable or not? is it rational and can it be good? After all, to study moralisation from a philosophical point of view is not only to describe or explain the effect, but to evaluate it in its epistemic as well as ethical dimension. Psychology as such does not have an answer, but it can help us understand through which mechanisms moralisation is generated. We will see that some, more than others, are assessable from a normative point of view.
One kind of mechanism, already described by Rozin (1999), is via a direct conceptual link with health. Health is a value in many cultures, and it may also happen that it becomes an overriding value; that is, it takes priority over other values, such as autonomy and solidarity, in specific social and historical contexts. This is the route recently explored by S. Joshua Thomas (2019) in criticising moralisation of health-related behaviours such as dietary habits. He claims that to prioritise health over other personal values, in some contexts of healthcare and care, should not be the default option. On a converging line, psychologist Suzanne Täuber (2018) explains that if health becomes moralised, society gets divided along the lines of citizens who conform to and citizens who deviate from the health-related moral norm. Moralisation via over-valuing health is a very interesting phenomenon in itself, but considered in its generality, it does not shed light on why some health-related products and not others become moralised, or more moralised than others, which is my concern here. For this reason, I will put it aside in my discussion.
Of the two other mechanisms that Rozin (1999) saw behind the process of moralisation of a health-related behaviour by an individual, one involves logically connecting the behaviour in question with a moral principle one already endorses. If one endorses the principle that harming others is morally wrong, and comes to believe that smoking harms other people, one will conclude that smoking is morally wrong. The same structure of argument can bring the conclusion that vaccination is morally good (and being an anti-vaxxer is morally wrong), as we saw in the brief discussion of Thomas’ example above. Here again, one of the premises is the moral principle that harming others is morally wrong. Notice that when the mechanism of moralisation takes the form of an argument, as in these cases, the attribution of moral properties to a health-related behaviour is justified. One can challenge the grounds of the justification by denying one of the premises, for example, that smoking does not harm others, or by downgrading the importance of the main moral principle with respect to others, such as autonomy. However, moralisation of health-related behaviours of this kind, though objectionable, emerges as the output of a rational process.
There is, however, another mechanism that Rozin (1999) considers as a possible explanation of moralisation, a non-cognitive one, which he calls affective-associative. This kind of mechanism is now extensively explored in psychological research (Rhee et al., 2019). It may involve emotions, typically disgust (Wisneski & Skitka, 2017). Think of someone who comes to consider eating meat as immoral after visiting a slaughterhouse, seeing how animals are killed, and feeling disgust and pain. Other studies show that the affective-associative mechanism can exist in the association of the moralised object with a person or an institution that was previously judged morally good or bad. This is the idea of moral contagion. Examples of this sort are sacred objects, such as a national flag or items that belonged to a saint or a hero. Cherishing or defending them can become highly motivating, while damaging or destroying them may be judged as morally outrageous. Likewise, objects associated with dictators or criminals (such as Hitler’s sweater) can become morally tainted (Tetlock et al., 2000).
The attribution of moral properties to objects can have a much flimsier basis, though. Jarudi et al. (2008) found that people can moralise any kind of everyday objects and products, such as refrigerators, coffee, vegetables, chairs, and mirrors. Specifically, in their study, refrigerators turned out to be judged as morally good. How can that be possible? The researchers suggested that this is due to our “tendency to automatically evaluate all stimuli on an affective level and to transform affective valence to moral valence” (p. 458). More specifically, they speculated that the familiarity of an object could be a predictor of its moral goodness, as familiar objects have an affective valence. Another possibility they mentioned is that the utility of objects may ground attributions of moral properties. They also found that older and politically conservative subjects had stronger moralisation tendencies—leaving the explanation of this finding to further research (and so will I). The important point to stress here is that the attribution of moral properties via this kind of associative route comes very cheap, so to speak, as it does not need a rational, justificative argument to back it. If refrigerators can be moralised in this way, then it is plausible that medicines can be as well.
Concluding this review of the mechanisms by which moralisation is produced, it is worth recalling the starting question: can the moralisation of a product or health-related behaviour be good, or bad, and in essence how can we evaluate it? I think there is no general answer. Knowledge of the production mechanism of the specific case of moralisation can be a guide for its evaluation, but only on a case-by-case basis. If the attribution of moral properties to a product or behaviour is logico-inferential, and one of the premises is a false belief, it can be concluded that that moralisation effect is epistemically not good. For example, if someone believes that obesity is immoral on the basis of the belief that obesity is caused by laziness and ill-will, and these are immoral traits, it may be answered that the moralisation is inappropriate because obesity is not caused by laziness and ill-will. This type of assessment, however, is more difficult for cases of moralisation with an affective-associative origin. We cannot simply conclude that the attribution of moral properties on the basis of emotions is irrational and therefore inappropriate—incidentally, the concept of rationality here should be defined more precisely. I believe that a more promising strategy for the evaluation of moralisation is to also consider its consequences. The normative dimension of philosophy can be either ethical or epistemic, so the consequences to be evaluated will be epistemic as well as ethical. Does moralising smoking have good ethical and epistemic consequences for public health and research? In this, philosophical reflection must go further than psychological research, which typically studies the effectiveness of moralisation in public health and its effects. We will return to the effects of moralisation by evaluating the case of HCQ in Section 5.
3 The HCQ case
In this section, I describe the main outlines of the controversy over the use of HCQ as a cure for Covid-19 to propose it as a case of moralisation of a medicine in the next section. The controversy over HCQ’s efficacy as a Covid-19 treatment ended with the results of two large randomised controlled studies in 2020, and as of 2022, scientific guidelines and healthcare authorities recommend against prescribing HCQ to Covid-19 patients (Harrington et al., 2021; WHO Solidarity Consortium, 2021). It started on March 17th, 2020, when an article was published in the International Journal of Antimicrobial Agents concluding that HCQ is efficient in clearing viral nasopharyngeal carriage of SARS-CoV-2 in Covid-19 patients in only three to six days (Gautret et al., 2020). The study followed the suggestion of a recent Chinese study on animal models and it was conducted on a small sample of 36 patients by a French team led by the microbiologist Didier Raoult, who is famous in France (Origgi et al., 2021). Had it been confirmed, the conclusion would have put an end to the global fear and, more than that, it would have done it with a cheap and familiar drug. HCQ, alongside chloroquine, has been prescribed since the 1940s as a cure for malaria. Its use has since been extended to rheumatoid arthritis, systemic lupus erythematosus, and other inflammatory rheumatic diseases (Schrezenmeier & Dörner, 2020). In 2020, its minimum cost was estimated as low as $0.08/day (Hill et al., 2020).
In the “unprecedented times” of the early months of the pandemic, as we used to say, the study sparked enormous interest in the scientific community, as well as in the public. When the paper was published, the promotion of HCQ as “the good drug” had already taken off because the results had been anticipated on Twitter. Immediately and from then on, US President Donald Trump endorsed the efficacy of HCQ in videos and public speeches, mostly from his Twitter account (Blevins et al., 2021). Trump emphasised that HCQ was cheap, that it was safe (because it has been prescribed in the US for decades, for other illnesses), that it could save lives immediately, and that people should have “the right to try” (Cathey, 2020; Facher, 2020). At the end of April 2020, the US Food and Drug Administration (FDA) authorised the emergency use of HCQ in the US for hospitalised Covid-19 patients (Manivannan et al., 2021).
In the meantime, Brazilian president Jair Bolsonaro insisted on recommending HCQ and ordered a massive production and import of the drug in Brazil. He appeared in videos with a bottle of HCQ pills on several occasions, and after he tested positive for Covid-19 in June 2020, he appeared in public showing the drug to the crowds like some sort of religious symbol (Casarões & Magalhães, 2021). The emotional response from the public went so high that a group of scientists, who published a study with a cautionary conclusion about the effectiveness of the malaria drug for Covid-19, received anonymous threats and abuse (Wessel, 2020).
In France, Didier Raoult, partially due to his previously earned scientific reputation and popularity, drew the attention of the media and the Government, even prompting President Francois Macron to visit Raoult’s lab in Spring of 2020 (Sayare, 2020; Sciama, 2020). When criticised for the lack of methodological rigor of his studies on HCQ, he defended himself by mentioning the Hippocratic Oath and the duty of beneficence. He presented himself as fighting against “the cold-blooded methodologists” with a drug that could save people’s lives (Berlivet & Löwy, 2020). As an effect of these and other endorsements of the efficacy of HCQ, in spring and summer of 2020, HCQ-based treatments were tested and prescribed off-label in many countries including France, Italy, India, the United States, and Australia. The market’s demand became so high worldwide that the WHO warned against the commercialisation of counterfeit HCQ products (Kim et al., 2020).
Let us now briefly consider the other side of the controversy. When it came out in the International Journal of Antimicrobial Agents, the study by Raoult and his team was also immediately criticised. Methodologists pointed out several flaws, including bias of loss to follow-up, anomalies in the reviewing process, and ethical concerns (Bik, 2020). The International Society of Antimicrobial Chemotherapy distanced itself from the paper (International Society of Antimicrobial Chemotherapy, n.d.). Anthony Fauci, the most visible member of Trump’s task force against Covid-19, declared the evidence in favour of the efficacy of HCQ “anecdotal”. On May 11, 2020, a case–control study on Covid-19 patients treated with HCQ, published in JAMA, disconfirmed the efficacy of HCQ and reported cardiac problems (Rosenberg et al., 2020). Meanwhile, supporters of evidence-based medicine kept urging that the main duty of a clinician is to do no harm, even in times when the pressure for action is strong (DeJong & Wachter, 2020; Zhai et al., 2020). Soon after, a very large cohort study appeared in The Lancet, concluding that HCQ increased mortality outcomes (Mehra et al., 2020). That could have been the end of the story, given that The Lancet is one of the most prestigious scientific medical journals, ranked at the top of its category, but in fact, the article was retracted. How could that happen? Let’s look at the case of the retracted article against HCQ in more detail.
The study (Mehra et al., 2020) claims to contain data from 96,032 Covid-19 patients obtained from 671 hospitals located on six continents. This data had been anonymised and aggregated by Surgisphere, an American company founded in 2008 by the second author of the article. The article was published on The Lancet website on May 22, 2020. It received numerous reactions from readers, one specifically signaling that the data presented for Australia were not compatible with those of the Australian health authorities. The article was therefore corrected on May 30, 2020, but the story was not over yet. Many researchers expressed doubts about the very possibility of collecting so much data in such a short time and on some of the results. An independent audit of the data was therefore requested by three of the four authors of the study and a letter was posted on the journal's website by the members of the editorial board (The Lancet Editors, 2020). Finally, the study by Mehra et al. (2020) was retracted; data were declared to be low quality and unverifiable. Moreover, a new policy for data quality was announced by the editors of the journal, according to which authors are now responsible for the verification of the data they present (The Editors of the Lancet Group 2020).
As a comment to the case, methodologists noted that the process of peer review and acceptance of the study had been too quick and much less careful than usual (Péretz et al., 2021). Supporters of the efficacy of HCQ, such as Raoult, suggested that political aversion to Trump and Bolsonaro was among the reasons why the Surgisphere data had been accepted without verification in the first place (Raoult, 2020). In fact, the editor-in-chief of The Lancet, Richard Horton, soon positioned himself openly against Trump’s decisions during the pandemic and published a book with his opinions (Horton, 2021). Horton defended the journal’s actions, saying that editors followed proper editorial processes and that the journal acted swiftly to evaluate and then retract the paper. However, in an interview with the magazine The New Yorker, he declared that peer review is not an effective system for detecting fraud because editors and reviewers typically trust that what they are reviewing is genuine research. He also denied that hype around HCQ had unduly influenced the editorial process for the HCQ study. Nevertheless, he consistently defined Covid-19 as a “moral provocation”, not just a health emergency (Knight, 2020).
4 Moralization of HCQ
In this section I intend to show that HCQ has been moralised by some prominent media and political figures, prominently Trump, Bolsonaro and Raoul. In the next section I will bring evidence to argue that this moralisation has had an effect on medical research, i.e. that it has leaked from the realm of public and political discourse to the more strictly scientific one. How these leaking mechanisms work is an interesting topic in the sociology of science, but one that I cannot develop here in full detail. One possible conceptual connection is this: moralization, as Paul Rozin has argued, produces media hype, and media hype tends to distort the distribution of resources in research, as Kristen Intemann (Intemann, 2020) has suggested—and as I will show in the case of HCQ in the next section.
It is important to note that I do not claim that the HCQ controversy can be appropriately accounted for in terms of moralisation only. In fact, it is a sociologically complex event, which can be described and assessed from the perspectives of epistemology, political discourse analysis, science communication, and ethics. There is already literature on the HCQ controversy at the intersection between medicine, ethics, and the philosophy of science. For example, Intemann (2020) described it as a case of scientific hype; that is when science communication exaggerates the benefits, or the evidence for those benefits, of particular theories, interventions, or technological products either explicitly or implicitly in a way that either obscures the risks presented by a technology or exaggerates its promise or benefits, given the evidence we have so far. Also, the concept of medical populism was applied to the HCQ case, described as “a political style that pit ‘the people’ against ‘the establishment’ using alternative knowledge claims to cast doubt on the credibility of doctors, scientists, and technocrats” (Casarões & Magalhães, 2021, 198). I propose that the HCQ controversy was also a case of moralisation of a medicine. Again, my goal is to elucidate what I take to be a useful concept by applying it to the recent case of HCQ, to which many other useful concepts plausibly apply, as well. In essence, I believe that the moralisation of HCQ is an effect that has contributed along with others to the peculiar media relevance and suboptimal characteristics of the research (but this is the subject of Section 5).
Let us now turn to the moralisation of the miracle drug by the already cited major figures in the media and political landscape, and consider positive moralisation first. A list of positive moral properties can be extracted from the arguments of the defenders of HCQ. Fairness is one, intended as distributive justice, or giving to everyone what they need and deserve. The low price of HCQ grounded this association. A second positive moral property is integrity. HCQ was presented as an already existing product, not tainted by the profit interests of Big Pharma. To support HCQ, in other words, could mean supporting honesty versus greed. The attributions of fairness and integrity to HCQ were part of Trump’s defence of the malaria drug.
Moreover, as we saw from Raoult’s defenses, HCQ was associated with benevolence, compassion, and the qualities of a good doctor. Readiness to help people and generosity were also evoked in Donald Trump’s tweets and declarations. To believe in the efficacy of HCQ could then become to be good at heart versus cold-blooded and uncompassionate (Fuhrer & Cova, 2020).
Finally, being morally good in the religious sense—being holy—was the moral property suggested by Bolsonaro’s rhetoric. “Holy” was the term he used in a letter thanking the Indian government for lifting the exportation ban on the drug (Casarões & Magalhães, 2021). Donald Trump made a statement on March 23th, 2020 that described HCQ as a “gift from God”. Patriotic goodness of HCQ was also present in some of Trump’s remarks (Cathey, 2020).
On the other side of the controversy, morally bad properties were associated with HCQ. Biasedness, absence of objectivity, and lack of scientific integrity were predominant. As a reverse effect of Raoult’s rhetorical use of “the good doctor” versus “the evil methodologists”, HCQ became a symbol of the disruption and even “suppression” of science (Abbasi, 2020). As HCQ was sponsored by Trump and Bolsonaro, the Democratic electorate in the US, and worldwide liberals in general, tended to associate HCQ with greed, dishonesty, and manipulation (Hart et al., 2020; Waksman, 2020). An opinion piece published in the British Medical Journal was titled “Donald Trump: a political determinant of Covid-19” (Yamey & Gonsalves, 2020). As true as this may sound, the title contributes to making HCQ not just a medicine, but a morally tainted product (see Section 2).
5 Effects on medical research
It could be suspected that the moralisation of HCQ has been a media and public debate phenomenon, but that it has had no effect on medical research. After all, Trump and Bolsonaro are not usually the heroes of virology and clinical researchers. Instead, as I will show in this section, there is evidence to conclude that the moralisation of HCQ did infect research—and with this value-laden verb, I am anticipating the conclusion, which is that the value contribution of moralisation in this case has had influence at the level of the integrity of medicine as a science. How has moralisation infected (or more neutrally, affected) medical research? I believe two levels can be isolated, to connect this case with the discussion of values in science that is being addressed in the philosophical debate today. First, and perhaps less surprisingly, the moralisation of HCQ has influenced at the level of the choice of research question. Moreover, the level of scientists' evaluation of the evidence has also been affected. Let us see both in more detail.
The moral importance of HCQ (good or bad) led many to engage in studies for or against the efficacy of the drug. As predicted by Rozin's model I illustrated above, moralisation produces scientific hype, i.e. focus of interest and polarisation of resources such as time and money. The abundance of these studies is documented by various sources (Yogendrakumar et al., 2022). A recent cross-sectional survey of registered trials shows that a very large number of clinical studies on HCQ for COVID-19 were initiated during the early stages of the pandemic, with a significant number still ongoing in November 2020 (Yogendrakumar et al., 2022). The large number of studies raised concerns about redundancy, as many of them had similarities with each other and with previous ones. The same review shows that the number of studies on HCQ went up immediately after Donald Trump's endorsement and the resulting media hype. This suggests that the value considerations behind the decision to deal with HCQ were not so much the generic personal convenience of securing easy publication—which may be found behind much Covid-science—but was more directly related to the perceived moral importance of the issue.
A clarification is in place here. Within the field of philosophy of science, it is important to recognize that the choice of research questions being value-driven is not inherently flawed, either from an epistemic or ethical standpoint. The discernment between legitimate and non-legitimate values in scientific inquiry remains an ongoing challenge, actively addressed by philosophers of science. In the specific context of HCQ research, however, it becomes evident that the impact of values on research decisions – specifically, the moralization—has yielded unfavorable outcomes. The widespread choice to extensively test HCQ resulted in two distinct ethical consequences. Small-scale trials on the effects of HCQ published in 2020 exhibited significant similarities to each other and previously completed and published research. Reproducibility of results stands as a critical aspect of high-quality scientific inquiry, where multiple studies affirming a finding enhance scientific confidence. However, conducting additional trials after a question has been definitively answered raises ethical concerns. This approach may assign patients to receive treatments that have already been proven ineffective, depriving them of the opportunity to explore potentially more beneficial alternatives. Secondly, the mass testing of HCQ led to an inequitable allocation of resources. With limited resources available, it is crucial to prioritize research endeavors that hold the highest potential for meaningful advancements. In the case of HCQ, the collective decision to extensively test its efficacy consumed valuable resources that could have been directed towards exploring other treatments or areas of research with greater promise.
The issue of unfair resource allocation in scientific research stems from the inherent limitations of resources, such as funding, personnel, and time. In any given situation, these resources are not unlimited, which means that allocating them to one research topic or problem leaves other important areas overlooked. The period from March to November 2020 serves as a notable example of this phenomenon, where the hype surrounding Hydroxychloroquine (HCQ) resulted in a polarization of available resources. This led to the proliferation of low-quality and redundant studies, potentially wasting valuable resources (Glasziou et al., 2020; Glasziou et al., 2020). Unethical implications arise from this skewed resource allocation, as medical research is commonly regarded as a public good that should be distributed fairly. The moralization of research topics exacerbates this issue by fueling hype and further polarizing resources, ultimately undermining equitable distribution (Intemann, 2020).
We come to the second way in which the moralisation of HCQ, through the generation of hype, caused the undue insertion of values into medical research. Considering HCQ good or bad altered the perception of inductive risk, i.e., it affected scientists' evaluation of the evidence. The problem with inductive risk is, in simplified terms, this: when can I risk drawing a conclusion from the evidence I have? The 'when' refers to the epistemic situation (how much certainty) but also ethical (what harm will come from a false positive and what from a false negative). If we think of the classic format of a scientific study in medicine, the question of inductive risk arises at various stages: how many patients is it sufficient to examine? in what way is it sufficient to examine them (control group or not)? how cautiously or confidently is it appropriate to express the conclusion when submitting for publication? Now, there is evidence that at all these stages inductive risk has been considered suboptimally in a large part of the scientific literature on the effects of HCQ. In the case of the very first study by Raoult and his team (Gautret et al., 2020), this was implicitly admitted by Raoult himself when he claimed that benevolence towards patients waiting for a cure is prior to methodology. What Raoult basically admitted was that the moral duty to do good (and to promote the “good” molecule) had influenced his assessment of the evidence; more specifically, he considered it sufficient for a positive conclusion regarding the effect of HCQ, justifying with value-intrusion a not insignificant inductive leap. It is difficult to judge what happened in the case of The Lancet's retracted article. Maybe the moral urge to block the HCQ campaign was part of the process that led to an overestimation of the quality of the Surgisphere data and quick acceptance and publication. Arguably, there is not enough evidence for a conclusion in this case, and I am not sure what kind of empirical research could adjudicate the issue. That being said, it remains a possibility that moral reasons to fight against HCQ, seen as morally bad, played some role.
Beyond these two egregious cases, but on which we cannot generalise, there is fortunately more robust data to support the claim that moralization of HCQ acted at the level of scientists’ assessment of evidence. Many of the studies conducted on HCQ before the large RCTs can be considered as biased inductive risk assessments. Some were too small, as they involved too few participants. Many were without a control group. This is unfortunately a hallmark of Covid-science but it is particularly visible in our case (Raynaud et al., 2021) (Jung et al., 2021). A systematic review gloomily states that
[a]t the design level, most studies lack the randomization, concealment of the generated sequence, and blinding/masking needed to generate sound evidence, when they are RCTs and not observational uncontrolled single-arm case series. At the analysis level, they lack the standard steps taken to minimize confounding such as prospective design, statistical adjustment for prognostic factors, (propensity) matching, or stratification […] Our examination has found the reporting to be very sparse and lacking the explicitness that is warranted, and the patient-important outcomes needed for decision-making are often not studied or not reported (Alexander et al., 2020), 123)
There is also a more technical point to consider in support of the hypothesis that the moralization of HCQ influenced the appreciation of evidence within the research community. It concerns the RCTs that have been authorised and then completed to settle the question of HCQ effectiveness. The methodology prescribes that an RCT can only be done when there is equipoise, i.e., doubt about the difference in effect between the new intervention and the standard one. The notion of equipoise is much debated, and some consider it unnecessary and confusing because it is difficult to operationalise. Whichever meaning of equipoise is used, however, it is difficult to argue that the HCQ case was one of genuine doubt. Several authors argue that when the RCTs were planned, there was already sufficient evidence that the treatment did not work (or insufficient evidence that it did work: the studies in favour almost all had some methodological flaws). Why then, forgetting equipoise, were these huge, expensive, and time-consuming RCTs authorised? Why, that is, did the researchers from large and prestigious institutions who proposed and designed these multicentre studies evaluate so little—so to speak—the already existing evidence? (Alexander et al., 2020). This too can be seen as a question of inductive risk: why was it felt that the already accumulated evidence was not enough? The moralisation hypothesis is one possible answer. Moralisation is a very strong motivator and showing that the “bad molecule” was ineffective (and thus vindicating good science) may have had the effect of passing over the equipoise requirement—paradoxically, at the expense of good science. Unfortunately, also to the detriment of ethics, since the motivation behind equipoise is to protect study participants.
The evaluation and thus the use and dissemination of evidence produced by others within the scientific community can also be altered by practical reasons, values, and biases. One of these is particularly interesting because it is directly related to moralisation. The “white hat bias effect” is defined as the manipulation of scientific results in favor of what is considered fair and ethical, often in the pursuit of improving health. This bias was first identified in the field of nutritional epidemiology and is believed to stem from the desire of scientists to act with integrity and improve public health. This can typically result in citation bias (preferential citation of studies with the “good” outcome), and institutional reports and press releases may present distorted information and make false claims about the effectiveness of interventions (Cope & Allison, 2010). An analysis of 437 studies on HCQ analyzed citation and found white hat bias effect (Bellos, 2021).
Misinterpretation of the results of others may be another aspect of the effect of moralising on the evaluation of evidence. A case-study analysis shows that three influential articles on HCQ as a treatment for COVID-19 that had numerically positive results (i.e., people in the treatment group did better on average), but not statistically significant ones, were misinterpreted as strong evidence against HCQ’s efficacy. As the author also points out, the meaning of the p-value is often misunderstood even by insiders: it happens that the lack of statistical significance is mistaken as proof that the tested hypothesis is false. However, his hypothesis is that a motivation of evidence bias cannot be excluded as an alternative to misunderstanding. The moral urgency to block the dissemination of pro-HCQ studies could in essence have motivated the jump from lack of statistical significance to false hypothesis. To clarify: while certainly a study with p-value above the threshold is not a good one to corroborate the effect of hcq, neither is it one to disconfirm the hypothesis (Hagen, 2022).
6 Concluding remarks
In the previous sections I introduced the concept of moralising health behaviour and extended it—in line with recent psychological research—to objects, in this case to a medicine, HCQ. I tried to show that in the first months of the pandemic, the attribution of moral properties to this molecule (by some very prominent scientific and political figures) infected the public and medical research itself. In particular, in the last section I provided evidence in favour of two theses: that the moralisation of HCQ acted as a value insertion at the level of research question choice, and at the level of inductive risk assessment by scientists. I also argued that in both cases the moralisation had no beneficial consequences from an epistemic or ethical point of view.
The latter assessment, however, is not generalisable to all cases of attribution of moral properties to medicines or interventions. As we saw in Section 2, after discussing the different mechanisms that can lead to moralisation, in order to assess moralisation we need to study the details of each individual case, its ethical and epistemic premises and consequences. Ethically, moralization is a double-sided sword, both useful and dangerous. To put it simply, the attribution of negative moral properties to smoking or excessive drinking, for example, can bolster the efficacy of public health campaigns aimed at dissuading people from such habits. The price, however, would be the stigmatisations of people who smoke or drink. Likewise, a recent study suggests contrasting effects of moralization of health interventions in how people estimate risks of zero-Covid versus more relaxed strategies adopted by national governments (Graso et al., 2021). In general, if we admit that the moral ought tends to be overriding, then researchers and scientific institutions should be aware of the effects of moralising topics, behaviours, or products in medicine and healthcare. Philosophers, sociologists, and psychologists can help scientists in detecting cases of moralisation and assessing them.
Where could this kind of research on the moralisation of medical interventions start from and how could it be conducted? A complete answer to this question would have to be developed in a separate work. However, I would like to suggest in closing this article some possible directions. First, if it is true, as I have argued, that moralisation produces hype, then instances of hype in the media can be seen as indications of moralisation. Media-analysis techniques are already available to detect hype. Psychological or text-analysis research could then connect the hype to the moralisation hypothesis, either by testing directly on people the attribution of moral properties to the object in question or by looking for these attributions in texts. Another effect of the moralisation of medicines and treatments is the increase in demand or, conversely, rejection and stubborn noncompliance. Again, these behaviours can be indications for an ongoing process of moralisation, which can be verified with psychological studies or textual analysis. When they happen, we should check for moralisation effects.
Moralisation can also manifest at the level of medical experts’ opinions, editorials, and opinion papers in leading journals, and possibly guidelines and institutional documents. In these cases, the phenomenon can be studied through qualitative methods such as discourse analysis and narrative reviews. Once individuated, moralization by experts could be overtly discussed within the scientific community with the help of philosophers and bioethicists, possibly with the involvement of a broader public, including all the relevant stakeholders.
Finally, although all the effects of product and treatment moralisation are resounding, and therefore worth studying, the difference between rational and discursive moralisation processes, on the one hand, and associative and emotional ones, on the other, can make a big difference, as suggested in Section 2. Moralisation may or may not be justifiable in the former case, while it is more difficult to assess it in the latter. Therefore, an important part of the study on moralisation in medicine should be to understand the mechanisms that make it happen, with the help of psychology and sociology. Overall, the identification and evaluation of moralisation of medicines and interventions is a problem that calls for genuine interdisciplinary research. I believe that this direction of research is as yet little explored by philosophers of science in general, whereas other aspects of value-intrusion in medicine and other sciences are already the focus of articulate reflection.
References
Abbasi, K. (2020). Covid-19: politicisation, “corruption”, and suppression of science. BMJ, 371, m4425. https://doi.org/10.1136/bmj.m4425
Alexander, P. E., Debono, V. B., Mammen, M. J., Iorio, A., Aryal, K., Deng, D., et al. (2020). COVID-19 coronavirus research has overall low methodological quality thus far: Case in point for chloroquine/hydroxychloroquine. Journal of Clinical Epidemiology, 123, 120–126. https://doi.org/10.1016/j.jclinepi.2020.04.016
Amoretti, M. C., & Lalumera, E. (2021). COVID-19 as the underlying cause of death: Disentangling facts and values. History and Philosophy of the Life Sciences, 43(1), 4. https://doi.org/10.1007/s40656-020-00355-6
Anderson, E. (2004). Uses of Value Judgments in Science: A General Argument, with Lessons from a Case Study of Feminist Research on Divorce. Hypatia, 19(1), 1–24. http://www.jstor.org/stable/3810929. Accessed 16 Mar 2022
Bellos, I. (2021). A metaresearch study revealed susceptibility of Covid-19 treatment research to white hat bias: First, do no harm. Journal of Clinical Epidemiology, 136, 55–63. https://doi.org/10.1016/j.jclinepi.2021.03.020
Berlivet, L., & Löwy, I. (2020). Hydroxychloroquine Controversies: Clinical Trials, Epistemology, and the Democratization of Science. Medical Anthropology Quarterly, 34(4), 525–541. https://doi.org/10.1111/maq.12622
Beswerchij, A., & Sisti, D. (2022). From Underground to Mainstream: Establishing a Medical Lexicon for Psychedelic Therapy. Frontiers in Psychiatry, 13, 870507. https://doi.org/10.3389/fpsyt.2022.870507
Bik, E. (2020). Thoughts on the Gautret et al. paper about Hydroxychloroquine and Azithromycin treatment of COVID-19 infections. Science Integrity Digest. https://scienceintegritydigest.com/2020/03/24/thoughts-on-the-gautret-et-al-paper-about-hydroxychloroquine-and-azithromycin-treatment-of-covid-19-infections/. Accessed 10 Apr 2022
Blevins, J. L., Edgerton, E., Jason, D. P., & Lee, J. J. (2021). Shouting Into the Wind: Medical Science versus “B.S. ” in the Twitter Maelstrom of Politics and Misinformation About Hydroxychloroquine. Social Media + Society, 7(2), 20563051211024976. https://doi.org/10.1177/20563051211024977
Brandt, M. J., Wetherell, G., & Crawford, J. T. (2016). Moralization and Intolerance of Ideological Outgroups. Routledge.
Bueter, A. (2022). Bias as an epistemic notion. Studies in History and Philosophy of Science, 91, 307–315. https://doi.org/10.1016/j.shpsa.2021.12.002
Bueter, A., & Jukola, S. (2020). Sex, Drugs, and How to Deal with Criticism: The Case of Flibanserin. In A. LaCaze & B. Osimani (Eds.), Uncertainty in Pharmacology: Epistemology, Methods, and Decisions (pp. 451–470). Cham: Springer International Publishing. https://doi.org/10.1007/978-3-030-29179-2_20
Casarões, G., & Magalhães, D. (2021). The hydroxychloroquine alliance: How far-right leaders and alt-science preachers came together to promote a miracle drug. Revista De Administração Pública, 55, 197–214. https://doi.org/10.1590/0034-761220200556
Cathey, L. (2020). Timeline: Tracking Trump alongside scientific developments on hydroxychloroquine. ABC News, 8. https://abcnews.go.com/Health/timeline-tracking-trump-alongside-scientific-developments-hydroxychloroquine/story?id=72170553
Cope, M. B., & Allison, D. B. (2010). White hat bias: A threat to the integrity of scientific reporting. Acta Paediatrica, 99(11), 1615–1617. https://doi.org/10.1111/j.1651-2227.2010.02006.x
DeJong, C., & Wachter, R. M. (2020). The Risks of Prescribing Hydroxychloroquine for Treatment of COVID-19—First, Do No Harm. JAMA Internal Medicine, 180(8), 1118–1119. https://doi.org/10.1001/jamainternmed.2020.1853
Douglas, H. (2009). Science, Policy, and the Value-Free Ideal. Pittsburgh: University of Pittsburgh Press. http://muse.jhu.edu/book/3730. Accessed 8 Jan 2022
Elliott, K. C. (2017). A Tapestry of Values: An Introduction to Values in Science. Oxford University Press USA.
Elliott, K. C., & McKaughan, D. J. (2014). Nonepistemic Values and the Multiple Goals of Science. Philosophy of Science, 81(1), 1–21. https://doi.org/10.1086/674345
Facher, L. (2020). Fact-checking Trump’s claims about hydroxychloroquine, the antimalarial drug he’s touting as a coronavirus treatment. STAT. https://www.statnews.com/2020/04/06/trump-hydroxychloroquine-fact-check/. Accessed 12 Apr 2022
Feinberg, M., Kovacheff, C., Teper, R., & Inbar, Y. (2019). Understanding the process of moralization: How eating meat becomes a moral issue. Journal of Personality and Social Psychology, 117(1), 50–72. https://doi.org/10.1037/pspa0000149
Foot, P. (1983). Moral Realism and Moral Dilemma. The Journal of Philosophy, 80(7), 379–398. https://doi.org/10.2307/2026455
Fuhrer, J., & Cova, F. (2020). “Quick and dirty”: Intuitive cognitive style predicts trust in Didier Raoult and his hydroxychloroquine-based treatment against COVID-19. Judgment and Decision Making, 15(6), 889–908. https://doi.org/10.1017/S1930297500008123
Fuller, J. (2021). What are the COVID-19 models modeling (philosophically speaking)? History and Philosophy of the Life Sciences, 43(2), 47. https://doi.org/10.1007/s40656-021-00407-5
Gautret, P., Lagier, J.-C., Parola, P., Hoang, V. T., Meddeb, L., Mailhe, M., et al. (2020). Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. International Journal of Antimicrobial Agents, 56(1), 105949. https://doi.org/10.1016/j.ijantimicag.2020.105949
Glasziou, P. P., Sanders, S., & Hoffmann, T. (2020). Waste in covid-19 research. BMJ, 369, m1847. https://doi.org/10.1136/bmj.m1847
Graso, M., Chen, F. X., & Reynolds, T. (2021). Moralization of Covid-19 health response: Asymmetry in tolerance for human costs. Journal of Experimental Social Psychology, 93, 104084. https://doi.org/10.1016/j.jesp.2020.104084
Hagen, K. (2022). Misinterpretation of statistical nonsignificance as a sign of potential bias: Hydroxychloroquine as a case study. Accountability in Research, 1–20. https://doi.org/10.1080/08989621.2022.2155517
Harrington, D. P., Baden, L. R., & Hogan, J. W. (2021). A Large, Simple Trial Leading to Complex Questions. New England Journal of Medicine, 384(6), 576–577. https://doi.org/10.1056/NEJMe2034294
Hart, P. S., Chinn, S., & Soroka, S. (2020). Politicization and Polarization in COVID-19 News Coverage. Science Communication, 42(5), 679–697. https://doi.org/10.1177/1075547020950735
Hill, A., Wang, J., Levi, J., Heath, K., & Fortunak, J. (2020). Minimum costs to manufacture new treatments for COVID-19. Journal of Virus Eradication, 6(2), 61–69. https://doi.org/10.1016/S2055-6640(20)30018-2
Horton, R. (2021). The COVID-19 Catastrophe: What’s Gone Wrong and How To Stop It Happening Again. John Wiley & Sons.
Howard, M. C. (2022). Are face masks a partisan issue during the COVID-19 pandemic? Differentiating political ideology and political party affiliation. International Journal of Psychology, 57(1), 153–160. https://doi.org/10.1002/ijop.12809
Intemann, K. (2020). Understanding the Problem of “Hype”: Exaggeration, Values, and Trust in Science. Canadian Journal of Philosophy, 1–16. https://doi.org/10.1017/can.2020.45
International Society of Antimicrobial Chemotherapy. (n.d.). Statement on IJAA paper | International Society of Antimicrobial Chemotherapy. https://www.isac.world/news-and-publications/official-isac-statement. Accessed 11 Apr 2022
Jarudi, I., Kreps, T., & Bloom, P. (2008). Is a Refrigerator Good or Evil? The Moral Evaluation of Everyday Objects. Social Justice Research, 21(4), 457–469. https://doi.org/10.1007/s11211-008-0082-z
Jefferson, T., Dooley, L., Ferroni, E., Al-Ansary, L. A., Driel, M. L. van, Bawazeer, G. A., et al. (2023). Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database of Systematic Reviews, (1). https://doi.org/10.1002/14651858.CD006207.pub6
Jung, R. G., Di Santo, P., Clifford, C., Prosperi-Porta, G., Skanes, S., Hung, A., et al. (2021). Methodological quality of COVID-19 clinical research. Nature Communications, 12(1), 943. https://doi.org/10.1038/s41467-021-21220-5
Kim, A. H. J., Sparks, J. A., Liew, J. W., Putman, M. S., Berenbaum, F., Duarte-García, A., et al. (2020). A Rush to Judgment? Rapid Reporting and Dissemination of Results and Its Consequences Regarding the Use of Hydroxychloroquine for COVID-19. Annals of Internal Medicine, 172(12), 819–821. https://doi.org/10.7326/M20-1223
Knight, S. (2020). The Lancet Editor’s Wild Ride Through the Coronavirus Pandemic. The New Yorker. https://www.newyorker.com/news/letter-from-the-uk/the-lancet-editors-wild-ride-through-the-coronavirus-pandemic. Accessed 12 Apr 2022
Manivannan, E., Karthikeyan, C., Moorthy, N. S. H. N., & Chaturvedi, S. C. (2021). The Rise and Fall of Chloroquine/Hydroxychloroquine as Compassionate Therapy of COVID-19. Frontiers in Pharmacology, 12. https://www.frontiersin.org/article/https://doi.org/10.3389/fphar.2021.584940. Accessed 12 Apr 2022
Mehra, M. R., Desai, S. S., Ruschitzka, F., & Patel, A. N. (2020). RETRACTED: Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: A multinational registry analysis. The Lancet. https://doi.org/10.1016/S0140-6736(20)31180-6
Mercuri, M. (n.d.). A pandemic of nonsense. Journal of Evaluation in Clinical Practice, n/a(n/a). https://doi.org/10.1111/jep.13750
Origgi, G., Branch-Smith, T., & Morisseau, T. (2021). Why Trust Raoult? How Social Indicators Inform the Reputations of Experts. Social Epistemology A Journal of Knowledge, Culture and Policy. https://hal.archives-ouvertes.fr/hal-03095293. Accessed 8 Mar 2022
Péretz, F., Bonini-Vuillod, J., Grivaux, M., Duracinsky, M., & Chassany, O. (2021). Littérature médicale et COVID-19: Comment trois articles ont influencé les médias et la décision publique en France. La Revue De Médecine Interne, 42(8), 583–590. https://doi.org/10.1016/j.revmed.2021.03.010
Raoult, D. (2020). Lancet gate: a matter of fact or a matter of concern. New Microbes and New Infections, 38, 100758. https://doi.org/10.1016/j.nmni.2020.100758
Raynaud, M., Zhang, H., Louis, K., Goutaudier, V., Wang, J., Dubourg, Q., et al. (2021). COVID-19-related medical research: A meta-research and critical appraisal. BMC Medical Research Methodology, 21(1), 1. https://doi.org/10.1186/s12874-020-01190-w
Repurposed Antiviral Drugs for Covid-19 — Interim WHO Solidarity Trial Results. (2021). New England Journal of Medicine, 384(6), 497–511. https://doi.org/10.1056/NEJMoa2023184
Rhee, J. J., Schein, C., & Bastian, B. (2019). The what, how, and why of moralization: A review of current definitions, methods, and evidence in moralization research. Social and Personality Psychology Compass, 13(12), e12511. https://doi.org/10.1111/spc3.12511
Rosenberg, E. S., Dufort, E. M., Udo, T., Wilberschied, L. A., Kumar, J., Tesoriero, J., et al. (2020). Association of Treatment With Hydroxychloroquine or Azithromycin With In-Hospital Mortality in Patients With COVID-19 in New York State. JAMA, 323(24), 2493–2502. https://doi.org/10.1001/jama.2020.8630
Rozin, P. (1999). The Process of Moralization. Psychological Science, 10(3), 218–221. https://doi.org/10.1111/1467-9280.00139
Rozin, P., & Singh, L. (1999). The Moralization of Cigarette Smoking in the United States. Journal of Consumer Psychology, 8(3), 321–337. https://doi.org/10.1207/s15327663jcp0803_07
Rozin, P., Markwith, M., & Stoess, C. (1997). Moralization and Becoming a Vegetarian: The Transformation of Preferences Into Values and the Recruitment of Disgust. Psychological Science, 8(2), 67–73. https://doi.org/10.1111/j.1467-9280.1997.tb00685.x
Sayare, S. (2020). He was a science star. Then he promoted a questionable cure for Covid-19. The New York Times, 13.
Schrezenmeier, E., & Dörner, T. (2020). Mechanisms of action of hydroxychloroquine and chloroquine: Implications for rheumatology. Nature Reviews Rheumatology, 16(3), 155–166. https://doi.org/10.1038/s41584-020-0372-x
Schwarz-Plaschg, C. (2022). Socio-psychedelic imaginaries: Envisioning and building legal psychedelic worlds in the United States. European Journal of Futures Research, 10(1), 10. https://doi.org/10.1186/s40309-022-00199-2
Sciama, Y. (2020) Is France’s president fueling the hype over an unproven coronavirus treatment? Science Insider News. https://www.science.org/content/article/france-s-president-fueling-hype-over-unproven-coronavirus-treatment. Accessed 11 Apr 2022
Solomon, M. (2015). Making Medical Knowledge. OUP Oxford.
Steel, D., & Whyte, K. P. (2012). Environmental Justice, Values, and Scientific Expertise. Kennedy Institute of Ethics Journal, 22(2), 163–182. https://doi.org/10.1353/ken.2012.0010
Stegenga, J. (2018). Medical Nihilism. Oxford University Press.
Tetlock, P. E., Kristel, O. V., Elson, S. B., Green, M. C., & Lerner, J. S. (2000). The psychology of the unthinkable: Taboo trade-offs, forbidden base rates, and heretical counterfactuals. Journal of Personality and Social Psychology, 78(5), 853–870. https://doi.org/10.1037/0022-3514.78.5.853
The Editors of the Lancet Group. (2020). Learning from a retraction. Lancet (London, England), 396(10257), 1056. https://doi.org/10.1016/S0140-6736(20)31958-9
The Lancet Editors. (2020). Expression of concern: Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis. The Lancet, 395(10240), e102. https://doi.org/10.1016/S0140-6736(20)31290-3
Thomas, S. J. (2019). Reconsidering the Moralization of Health: Practices Versus Concepts, and What We Can Learn from Evidence-based Research. Cambridge Quarterly of Healthcare Ethics, 28(02), 215–224. https://doi.org/10.1017/S0963180119000069
Waksman, R. (2020). COVID-19: Leave politics out of practicing medicine. Cardiovascular Revascularization Medicine, 21(8), 937–938. https://doi.org/10.1016/j.carrev.2020.05.005
Wessel, L. (2020). ‘It’s a nightmare’. How Brazilian scientists became ensnared in chloroquine politics. Science Magazine. https://www.sciencemag.org/news/2020/06/it-s-nightmare-how-brazilian-scientists-became-ensnared-chloroquine-politics
Wisneski, D. C., & Skitka, L. J. (2017). Moralization Through Moral Shock: Exploring Emotional Antecedents to Moral Conviction. Personality and Social Psychology Bulletin, 43(2), 139–150. https://doi.org/10.1177/0146167216676479
Yamey, G., & Gonsalves, G. (2020). Donald Trump: a political determinant of covid-19. BMJ, 369, m1643. https://doi.org/10.1136/bmj.m1643
Yogendrakumar, V., Dewar, B., McGuinty, M., Dowlatshahi, D., Dyason, C., Kwok, E. S., et al. (2022). Many trials of hydroxychloroquine for SARS-CoV-2 were redundant and potentially unethical: An analysis of the NIH clinical trials registry. Journal of Clinical Epidemiology, 143, 73–80. https://doi.org/10.1016/j.jclinepi.2021.11.011
Zhai, M. Z., Lye, C. T., & Kesselheim, A. S. (2020). Need for Transparency and Reliable Evidence in Emergency Use Authorizations for Coronavirus Disease 2019 (COVID-19) Therapies. JAMA Internal Medicine, 180(9), 1145–1146. https://doi.org/10.1001/jamainternmed.2020.2402
Acknowledgements
The first idea of this paper was presented at EPSA 2021, in the symposium “COVID-19 in the public sphere: conspiracies, exceptionalism, and moral profiling”. I would like to thank all the participants and attendees. Two anonymous reviewers from this Journal also contributed significantly to the initial version's improvement.
Funding
Open access funding provided by Alma Mater Studiorum - Università di Bologna within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
Single author.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Informed consent
None Applicable.
Financial or non-financial interests
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lalumera, E. Moralisation of medicines: The case of hydroxychloroquine. Euro Jnl Phil Sci 13, 39 (2023). https://doi.org/10.1007/s13194-023-00542-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13194-023-00542-9