Abstract
The field of Neuro-Engineering seems to be on the fast track towards accomplishing its ultimate goal of potentially replacing the nervous system in the face of disease. Meanwhile, the patients and professionals involved are continuously dealing with human bodily experience and especially how neuro-engineering devices could become part of a user’s body schema: the domain of ‘embodied phenomenology’. This focus on embodiment, however, is not sufficiently reflected in the current literature on ethical and philosophical issues in neuro-engineering. In this article we will focus on this lacuna by explaining existing data on neuro-engineering user’s experiences by using phenomenological concepts such as transparency and the concepts that may facilitate this: functionality, sensorimotor feedback and affective tolerance. By introducing and applying these concepts to four real life case examples, we will discuss practical implications and guidelines which can contribute to the actual success of incorporation of the device by the patient. First, we will discuss the importance of a ‘Patient Preference Diagnosis’ (PPD), which can serve as a way to prepare the patient for the existential reorientation involved in the process. In addition, a Patient Transparency Diagnosis (PTD) during and after such a process is also relevant when wanting to provide the medical field in general with feedback, and the patient in particular with possibilities to fine-tune the device. From these practical guidelines we will conclude that the phenomenological approach can be very valuable when applied to the field of neuro-engineering.
Similar content being viewed by others
Introduction
The 1974 movie The Terminal Man paints the picture of a scientist who implants himself with a brain-implant hooked up to a computer in order to counter the seizures he experiences. Back then this was marked ‘Sci-Fi’. A little over 40 years later, Nature publishes one of the first successful case reports involving a brain-computer interface (BCI), restoring the communicative abilities of a patient with severe Amyotrophic Lateral Sclerosis (ALS), a muscle and nervous system disorder, which ultimately leads to complete isolation due to loss of muscle function [1]. In the same year, a group in Switzerland [2] succeeded in restoring the walking pattern in two primates with paraplegia by implanting a spinal cord stimulator, which translated walking pattern signals in the brain to actual motor response.
With these latest accomplishments, the field of Neuro-Engineering, seems to be on the fast track towards its ultimate goal of replacing the nervous system. Neuro-engineering or ‘Neural Engineering’ involves the process of repairing, restoring, replacing, or bypassing the nervous system with the aim of implementing solutions to problems associated with neurological limitations and dysfunctions, for example in the face of disease [3]. For the patientsFootnote 1 in question, these interventions often mean a step towards a life that healthy people take for granted. In addition, these interventions often also ask a patient to incorporate a ‘strange’ body, initiating a process of embodiment which takes a different form in every patient. As such, neuro-engineering is continuously dealing with human experience, both of the patients involved, as well as the family and friends surrounding the patients, and to a certain extent, even the doctors and technicians supporting the patients through the process.
In recent literature in the field of neuro-engineering research, the importance of user-centered design in e.g. BCI development is being promoted [5,6,7,8]. However, neither this literature, nor the philosophical and bioethical literature on neuro-engineering in general, seem to focus on the aspect of bodily experience. In a scoping review performed by Burwell et al. [9] looking into the current key issues associated with BCI use, the authors report the most frequently cited issues to include user safety, justice, privacy and security. Issues of incorporation and the effect of BCI use on human experience were not among these issues. When we look at how issues regarding human experience and neuro-engineering are discussed in the literature, we notice that many other aspects than ‘embodiment’ are brought forward. Many articles focus on the potential effect of neuro-engineering devices such as BCIs or Deep Brain simulation (DBS) on personality or autonomy [10,11,12,13,14,15], often ignoring the more physical component of tool incorporation. What is more, of the articles that do zoom in on embodied tools, such as the article by Heersmink [16], many present with a rather negative connotation, focusing on the current limitations of devices such as BCIs and the current lack of possibilities for incorporation.
So, although there is no lack of sensitivity to user experience within the field of neuro-engineering research, the focus on the bodily aspect of the user experience, remains close to non-existent [17].
A field that does pay attention to human experience and to the way in which external tools may be incorporated in a person’s body schema is that of phenomenology, and especially the theoretical framework of ‘embodied phenomenology’. An important question here is how and to what extent a neuro-engineering device is a tool or can be incorporated as a part of the ‘self’ [16, 18].
In this article, we aim to explain existing data on neuro-engineering users’ experiences in terms of phenomenological theory. We will start out by exploring the phenomenological concepts of interest to the field of neuro-engineering, after which we will apply these phenomenological concepts to the practice of neuro-engineering, in parallel to philosophers such as Jenny Slatman [19] who have applied phenomenological concepts to medical interventions in general. For this purpose, we will introduce a total of four case examples (Mrs. A, Mr. B and two patients as interviewed previously by Dalibert [20]). Finally, we will discuss practical implications and recommendations which can be of benefit to the field of neuro-engineering.
Four Case Examples – Ms. A, Mr. B, Mr. van Houten and Mrs. Bloemen
Ms. A
Ms. A is a real patient, who became world-famous when she received a BCI from a neuroscientific research team in Utrecht which allowed her to spell on a computer screen by using her brain waves [1]. At the time of the informed consent, Ms. A was 58 years old and in a locked-in state due to her disease [1, 21, 22].
During brain surgery, the researchers placed electrodes of the motor cortex of Ms. A. What then followed was an intense training period of 28 weeks. The electrodes placed over the cortile motor movement area of the brain, were hooked up to a decoding software. By continuously performing training tasks, which entailed withholding or activating ‘brain clicks’ on a computer screen, the software would get used to interpreting the meaning of particular signals in the brain activation of Ms. A. On day 197, the software was accurate enough at decoding Ms. A’s brain signals: Ms. A could use the spelling system as an autonomic form of communication.
Mr. B
Mr. B is also a real-life patient who participated in one of the first experiments using the technique of epidural stimulation, a form of spinal cord stimulation (SCS) [23, 24]. Mr. B injured his spinal cord after a severe vertebral fracture due to a car accident. This left him with a motor complete paraplegia of the legs.
In the experiment, Mr. B received an electrode with 16 contacts which goes over the lower spinal cord. A continuous electrical current at different frequencies and intensities is applied to specific locations on the lower part of the spinal cord, activating nerve circuits. After months of intense training in combination with the epidural stimulation, Mr. B was able to voluntarily retract and extend his legs, bend his knees, and stand with assistance of a cane.
Mr. van Houten and Mrs. Bloemen
Mr. van Houten (61 years old) and Mrs. Bloemen (45 years old) are two real-life patients interviewed in a case series by Dalibert [20] looking into patient experiences while ‘living with spinal cord stimulation’. Both patients received epidural SCS, in their case for the indication of chronic pain, for Mrs. Bloemen due to diabetic neuropathy, for Mr. van Houten due to failed back surgery syndrome. The implanted electrodes are similar to those used for Mr. B and implanted surgically over the area of the spinal cord related to the patient’s specific pain perception. The electrical current applied to the spinal cord modulates the pain signal, allowing the pain perception to be interrupted.
While for both patients the stimulation technique has led to a significant reduction in pain perception and increase in independence and mobility, they both experience the neuro-engineering device significantly differently. As we will see, this has implications for medical practice.
Phenomenology: the Embodied Experience and Body Boundaries
Neuro-engineering touches upon the human experience of body-ownership and ‘ownness’Footnote 2 in general. By introducing technical devices which aim to recover some of the ‘natural’ abilities healthy subjects have, neuro-engineering asks of the patients to somehow ‘recalibrate’. This emphasis on experience fits well into the philosophical tradition of phenomenology. Phenomenology has sought to unravel what in the literature is called Erlebnis, our lived experience of the world, our body, and others [19]. According to German philosopher Edmund Husserl, the founder of phenomenology, consciousness makes it possible for humans to be more than just a passive receiver of stimuli. While sensations (Empfindungen) are only the raw matter, consciousness allows us to ‘grasp’ (auffassen) a whole object or situation. This ‘grasping’ is also called the ‘intentionality’, the fact that consciousness is always being conscious of ‘something’ [19]. As such, phenomenology focuses on how things appear to us instead of how things ‘really are’ [19]. We might see a simple screen with spelling software, but the same screen could to Ms. A appear as his/her voice, the only way to interact with the world. And similarly, a broken screen to Ms. A might mean something completely different than to the technician called in to fix it.
Mr. B, after having lost his ability to walk, is left with two legs still similar to the ones which used to help him around, but now ‘not functional’. It is this loss of functionality which leaves the patients with a pair of dull legs, they, as studies suggest often feel alienated towards [26] or disconnected from [27]. What is more, over time the legs will lose their original shape due to muscle atrophy, making recognition even more difficult.
This makes one wonder what it is that makes us able to claim body ownership at all. What is considered my ‘own’? The many different theories in the literature on this subject show us that answering this question, often also implies answering questions on identity. Some, such as the psychologist Baumeister [28], claim that ‘your own’ is all that is held together by your skin, as such arguing for a view of the self as a ‘bodily self’. Although patients such as Mr. B undergo changes, which leave them with non-functional legs, the integrity of the body is still intact. The skin the patient ‘lives in’ is still intact, as the same ‘skin-encapsulated ego’.
Some, mostly scientific researchers, claim that everything that ‘contributes’ to your body is yours. In contrast to the previous theory, functionality plays an important role here:
“We propose that the self-attribution of an entity may be determined, not just by its physical features, but by whether the entity can afford actions that the brain has associated with the limb which it replaces.” (p.31) [29]
In the case of paraplegia, this theory would leave the patient with a great lack of ownership, given the fact that paraplegia per definition leads to an enormous lack of functionality.
Embodied Tools, Body Schema’s and Transparency
While the body undergoes tremendous changes throughout a lifetime, both due to natural process of aging, as well as more externally mediated changes such as trauma leading to SCI, most of us manage to continuously identify ourselves with the changing body. We cut our hair, add clothing and accessories, we observe new wrinkles on our face, and we might need time to get used to them, but eventually we continue to identify them as ‘ours’. Human beings also use body extensions, like clothing and tools. It is especially this latter category of extensions that the field of neuro-engineering is focused on developing. The question is: can human beings come to understand these tools as part of themselves, as part of their body? Can they come to experience and recognize them as part of their selves, as ‘own’?
In his essay Embodied Tools, Cognitive Tools and Brain-Computer Interfaces Richard Heersmink [16] discusses the phenomenological consequences of some of the earliest forms of BCIs and especially to what extent these neuro-engineering tools are incorporated into the ‘body schema’ of the patients and as such could be considered embodied tools. ‘Body schema’ is a term often used by French philosopher Merleau-Ponty, who is known for his notion of ‘embodied’ consciousness. For Merleau-Ponty, the previously discussed notion of intentionality, ‘giving meaning to that which appears and manifests itself’ (p.66) [19], is a bodily affair. This intentionality functions without one really being aware and is a key element of the ‘body schema’. The basis of this schema follows from a coherence or unity at two different levels:
-
1.
The parts of the body form a unity that does not just result from their sum total: the living body is experienced as one, rather than as a torso with a head, two arms and two legs attached to it.
-
2.
In its pre-reflective perception and acting, the relationship between our body and the world is not oppositional but marked by interaction and harmony.
Don Ihde defines a body schema similarly as ‘a non-conscious neural representation of the body’s position and its capabilities for action’ (p.6) [16]. Whether or not tools have the possibility to be incorporated into the body schema depends on the so called ‘transparency’ of the tools. Martin Heidegger’s distinction between Zuhanden (ready-to-hand) and Vorhanden (present-at-hand) illustrates this idea of transparency. Let’s take for example a hammer. To someone who has never used a hammer before, the tool might feel clumsy, and that person is focused on learning how to work with the tool. As such the tool demands attention, remains in the forefront and is ‘present-at-hand’. To someone having used a hammer before and being able to use it properly, it becomes a true tool, a means with which he can accomplish his aims. As such, using the tool of a hammer is no longer a point-of-focus, requiring conscious thought about how to use it, where to hold it, and so on. Don Ihde builds further on this by stating that when using embodied tools to interact with the environment, one does not first intend an action on the tool and then on the environment. Rather, ‘one merely intends an action on the environment through the tool and does not consciously experience the tool when doing so. The perceptual focal point is this on the tool-environment interface, rather than on the agent-tool interface’ (p.6) [16]. This incorporation takes time, sometimes years as it will in the case of Ms. A for example, before a patient is truly able to use the tool properly.
Heersmink [16] mentions two properties of tools which are beneficial to transparency and as such, embodiment. First of all, he describes how trust in a tool is necessary for embodiment. If we use the example of a hammer, one that is stable, in which the handle does not have the tendency to fall off, will be incorporated more quickly than one which shows a variable performance. Second, and quite interestingly, Heersmink [16] discusses the role of proprioceptive feedback. As we briefly discussed in the case of Mr. B, proprioceptive feedback is the sensory information one receives as a result of a certain movement, and that healthy subjects mostly take for granted. If we walk, we feel the earth under our feet, if we slam a hammer on a nail, we feel the backlash of the force and so on. According to Heersmink [16], this feedback is necessary while using tools in order to be able to assess the effect the tool has had on the environment and the agent. More trust in a tool and better proprioceptive feedback from it, increase the ease with which they can become transparent to the user and hence, embodied.
Functionality, Proprioceptive Feedback and Affective Tolerance
Jenny Slatman [19] in her book ‘Our strange Body’ reaches similar conclusions to Heersmink [16]. When looking at what might help a patient tolerate and embody ‘the Strange’, regain of functionality and through that trust in the tool, as well as the presence of proprioception or sensory feedback are important. However, Slatman adds in a third and more difficult concept that in her opinion plays a role in the embodiment process: emotional or affective tolerance. Jenny Slatman explains this concept by introducing the example of hand transplantations. In general, hand transplantations are considered successful, both in the eyes of the patient as well as the doctor, when functionality has been regained. However, there are examples of patients who received single hand transplantations which too regained almost full functionality after the transplantation, with almost no visible scarring or color differences. However, these patients do not reach the state of phenomenological unity as the ‘successful’ transplant patients do with a similar level of functionality. Even though functionality is intact, these patients explained to still feel a great distance to the hand and how it looked on their body. In fact, some of these patients even opt to amputate the transplanted hand not too long after the initial surgery. As Slatman explains, we cannot expect everyone to incorporate ‘the Strange’ as easily. According to Slatman, examples like these make clear the fact that regain of functionality in itself, and as such incorporation in the body schema itself, are necessary but not sufficient developments when it comes to the process of incorporating ‘the Strange’. Rather, emotional or affective tolerance is necessary. Through this last remark, Slatman also points out the components missing in theories of philosophers such as Merleau-Ponty, whose theory on the body schema needs to be supplemented as his analysis merely starts from ‘handiness’ and functionality.
These three aspects can be further illustrated by applying them to our case examples. In the case of Ms. A, almost all functionality is lost. As such, for neuro-engineering to be able to bring back the level of functionality of these patients to completely normal, a lot needs to happen. The BCI of Ms. A, however, focuses on one subset of problems, namely that of communication. We could say that this new BCI succeeds in its mission: as one of the first and most advanced devices in the world, it allows Ms. A to use her computer to communicate her thoughts and wishes. However, as one can imagine the device has its limitations. Speed, accuracy and complexity of language are not at the same level as it once was. The question now is, to what extent does this influence Ms. A’s ability to ‘tolerate’ this external tool, this ‘Strange’?
Secondly, we have the point of sensory feedback to address. Interestingly enough, in the case of the BCI of Ms. A we cannot really speak of sensory feedback, other than the indirect visual feedback received by seeing the spelling screen. By using the typing software, Ms. A is able to communicate to the outside world. However, the process of typing, and the success of doing so, is not something Ms. A experiences physically, as she would when for example opening and closing her mouth to speak and hearing her voice in the process. Rather, the feedback is indirect, just as we receive feedback when correcting a text we have written down on the computer. Perhaps we could argue, the feedback has mostly occurred during the training period, where Ms. A was performing multiple tasks per day in order to adjust the software to her own personal ‘brain-waves’.
Lastly, the need for affective or emotional tolerance for ‘the Strange’, which might be difficult if not impossible in BCIs. Unlike the previous example of hand transplantations, which in their exterior mimicked hands, the BCIs such as used by Ms. A do not have an exterior easily identifiable as a body part or even human tissue. Will a patient ever really tolerate this? On the other hand, we have also discussed examples of other inanimate tools, which have proven to be possible to incorporate in the body schema. Hammers, glasses, hats, we have been able to look beyond these and use them as tools within our body schema. Therefore, in the case of neuro-engineering, we might expect the same.
Now let us take a closer look to Mr. B, our patient with paraplegia. If we again apply the criterion of functionality, we could say that indeed, the neuro-engineering device is one which delivers to a certain extent. Under stimulation and due to the brain implant which uses the brain’s own waves as an initiation for the walking pattern, the patient would be able to stand in an upright position and move about in a reasonably smooth manner. Other aspects of the spinal cord injury however, such as bladder control or pain experience, are not necessarily addressed or tackled by the current neuro-engineering devices. Intuitively, we might think that the regain in motor response in itself could be a valuable addition to the quality of life of the patient. However, for many patients the lack of mobility itself is not the major concern. Rather, the limiting problems of bladder control, but also the extreme pain and spasticity due to the injury, often have priority for the patient [30, 31]. We might therefore wonder whether the functionality we aim for at first glance, is indeed the type of functionality that matters for the patient.
The point of proprioceptive feedback is a difficult one. The concept of feedback is of course very important in the process of locomotion. Any movement in our legs leads to a change in our muscles, which in their turn fire to communicate their position and strength. Due to this, locomotion continuous to be a smooth, synchronized movement. Therefore, scientists have always been interested in incorporating feedback in their neuro-engineering devices. One of the first successful spinal cord stimulators in paraplegic monkeys indeed contained a sensory feedback component, by recording the dorsal roots in the spinal cord (which are responsible for gathering all the sensory feedback information coming from the hind limbs) and feeding this info back into the spinal cord stimulation processor, which activates and steers the locomotion pattern.
However, this feedback in itself is interesting. Unlike feedback in a healthy physiological state, the neuro-engineering device does not allow for the conscious awareness of feedback for the patient. As we discussed, sensory feedback in the form of proprioception in a healthy subject is often an unconscious process. We are for example not continuously made aware of the fact that our feet are touching the ground. Only when the situation changes, and we suddenly feel ‘the ground falling from under us’, we are suddenly forced to pay attention to the sensory feedback which was once doing its job in silence. In the case of feedback of these neuro-engineering devices, however, the feedback is only fed back into the processor, which creates the algorithm for the walking pattern. This processor bypasses the spinal cord injury, as well as the possibility of conscious awareness for the patient. As such, the functional use of feedback remains intact, but the felt experience of feedback is lost.
Lastly, the point of affective tolerance. In the example of Mr. B in particular we have an interesting situation: a device which provides electrical current takes over the locomotion of the patient. One would consider that to be perhaps quite a severe intervention. However, on the outside we might see little sign of such an intervention. Unlike the external screen in the case of Ms. A, Mr. B will have a device implanted dorsally to the spinal cord and epidural space, which except for some scars from the surgery, and the contours of the implanted battery, will show little else on the outside. The most important question in this setting then becomes, does that make the tolerance easier? If one is able to forget the device by actually not seeing the device?
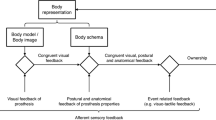
To summarize, we have discussed a total of three concepts which influence transparency, leading to embodiment through incorporation in the body schema (see Fig. 1). We have defined these factors based on previous literature applying these concepts deduced from phenomenological philosophy to real-life neuro-engineering users’ experiences [16] or other medical interventions in general [19]. In addition, we have shown how these concepts can be used to explain user experiences in two typical case examples, Ms. A and Mr. B. However, it could be questioned whether these factors draw a complete picture of all factors involved in transparency. One potential point of discussion could be the factor of affective tolerance, which unlike the other two factors, seems to allow for more interpretations, as we will see in the next section. It would be fruitful to further consider the possible subfactors which form the broader factor of affective tolerance, perhaps using additional methods such as qualitative empirical studies, to add to the current phenomenological approach.
In addition, the fact that we position ‘incorporation’ as the ultimate goal in this paper is based on the idea that the neuro-engineering device aims first and foremost to repair and restore functionality to a basic functioning level, as close to ‘normal’ as possible. Any part of normal functioning when using our body as ‘a tool’, is the level of transparency we reach with our body. As previously discussed in the examples of the hammer as a tool, transparency allows us to perform the task without being focused on the tool itself, making the task easier. Therefore, it is not strange that a team of engineers, doctors together with the patient often wish to reach a state of transparency.Footnote 3 Is this really necessary? Could we do without? Well, the examples we have discussed of the current state of most neuro-engineering devices already show us that, although we are still far from a level of transparency we can reach when using a hammer, these devises are still tremendously helpful for the patients using them. Therefore, a neuro-engineering device can definitely work without reaching a full level of transparency. However, as we have also discussed earlier, reaching full transparency, and as such being able to ‘ignore’ the device while using it, makes the device as much a port of your ‘normal’ body as the original, now malfunctioning, body part. For the acceptance, or incorporation, of such a device into the rest of the body and the patient’s life as a whole, we believe that to be a huge benefit.
In order to be able to apply the previously theoretical concepts in the heterogeneity of practical clinical life, we will zoom in on some practical implications and guidelines in the next section.
Practical Implications and Guidelines
If applying the three concepts important for transparency to two real-life case examples has taught us one thing, then it is that there is an enormous amount of heterogeneity in how and to what extent these concepts apply. We have seen how functionality in cases such as those of Mr. B can be a point of debate: is the functionality gained by a SCS stimulator for motor response really the type of functionality a paraplegic patient is aiming for? Also, we have seen how sensory feedback, although present, does not necessarily create more transparency or eases the incorporation of the implant in the body schema. In addition, when comparing Ms. A to Mr. B, we have also discussed how emotional or affective components play a role in our tolerance of neuro-engineering devices. Although we might expect Ms. A to have more difficulty in accepting the software required for communication, as it works through an always present computer screen, patients with an implantable device such as Mr. B also present with emotional difficulty to accept the implant, even though they are not clearly reminded of the implant. Another illuminating example of heterogeneity can be found in the previously discussed series of patient interviews published by Dalibert [20]. Dalibert brings forward two contrasting examples. First of all, Mrs. Bloemen is introduced, about whom Dalibert states the following:
“Visually, haptically and affectively Mrs. Bloemen cannot relate to or identify with the SCS. As she can see and touch the pulse generator under her skin she cannot identify with and incorporate the neuromodulation technology. It remains a tool or an instrument; it is not (a) part of her body” (p.650) [20].
In contrast to Mrs. Bloemen, Mr. van Houten states the following about his SCS experience:
“Mr. Van Houten is grateful for the neuromodulation technology that has not only become part of his body but has also enabled him to do things and to be part of the world –of life- again. In fact, he is so content with it that, as he told me later in the interview, he would like to have a zipper put in his back so that the world could see his implant, which he calls a pacemaker for his legs and back”. (p.641) [20]
So, a similar device with a similar position within the body and with similar functionality and sensory feedback, leads to a very different experience between two patients. In Mr. van Houten’s case, we could state that the implant is completely incorporated in the body schema and transparent to such an extent, that the patient himself wishes it would be more apparent with the help of a ‘zipper’. Comparing the two cases tells us that transparency in the case of Mrs. Bloemen seems to be unrelated to functionality, unrelated to sensory feedback as such, but an affective or emotional issue, related to the patient and its specific being-in-the-world. Dalibert [20] goes on to explain how for Mrs. Bloemen, not only her own view on the implant, but especially that of her husband is crucial for the experience of transparency. She states:
“I don’t like it that he [her husband] can feel it. At first you make jokes about it but at some point the fun stops.” (p.650) [20]
Not only does this statement illustrate the lack of transparency in Mrs. Bloemen’s particular case, but also the fact that Mrs. Bloemen is very much focused on what Merleau-Ponty defined as ‘Body Image’. Gallagher [32] describes the concept of ‘Body Image’ as follows:
“[...] an intentional content of consciousness that consists of a system of perceptions, attitudes, and beliefs pertaining to one's own body”. (p.149) [32]
Instead of incorporating the device into the body schema and allowing it to disappear as any truly functional tool would, Mrs. Bloemen is ‘stuck on’ the ‘Body Image’ of the device, making it hard to truly accept ‘the Strange’. We could state that this notion of ‘Body Image’ is an influencing factor for the concept of affective tolerance, as depicted in Fig. 1. Whether or not a patient will turn out like a Mrs. Bloemen is a difficult prediction to make beforehand. It requires careful consideration and conversation, allowing the patient to draw up possible scenarios involving neuro-engineering devices, their consequences, and the patient’s ability to accomplish the existential reconstruction necessary to leave the stage of ‘body-image focus’, allow for affective tolerance and reach transparency. What this boils down to is the fact that the experiences of patients with regard to the ‘embodiment’ of a BCI can be very different, even if many of the factors that facilitate embodiment such as functionality are present. That is exactly why phenomenology can be useful in a collaboration with neuro-engineering.
Patient Preference Diagnosis
In the last decades, medicine has come to realize more and more that patient preferences should be reckoned with in making treatment decisions, and informed consent and shared decision-making are concepts that are nowadays prominent in medical research and practice. In an editorial comment in the British Medical Journal (BMJ) [33] Godlee has made a plea for a ‘new’ form of diagnosis, named the ‘Patient Preference Diagnosis’ (PPD). In the absence of such a PPD:
“The doctor recommends treatment based on what is known of the patient’s disease, age, and general health, and using evidence on which treatments work best, but fails to discover what matters most to the patient” (p. 7745) [33].
An important goal of the PPD is to draw a ‘map’ of the patient’s wishes, values and norms, as well as for example the patient’s vision on his or her body. Part of the PPD conversation is to draw out the scenarios of life after neuro-engineering interventions and possible consequences of each scenario within a patient’s life to come to an understanding which is as well-rounded as possible. When applying this to clinical neuro-engineering, we could say that any neuro-engineering endeavor requires a great deal of PPD before even starting the process. But more than that, it requires continuous attention during and after the process of implantation, training etc. What neuro-engineering in combination with phenomenology has taught us, is although we can formulate concepts that are important in the process of neuro-engineering, it boils down to the patient in specific to come to the conclusion whether and how the device is incorporated in the body schema and leads to a comfortable degree of transparency. It requires a form of existential reorientation.
Although this focus on inquiring information on patients’ preferences is already an important part of the shared decision-making effort in the clinic, it is far less common to inform, inquire and discuss about the bodily experiences of a patient in relation to an intervention. This lacuna is exactly the reason why the phenomenological approach can be very valuable when applied to the field of neuro-engineering.
Although doctors have experience in how to introduce their patients to concepts such as an implant, a stimulator, an electrical wire and so on, understanding what is going to happen and trying to picture what the experience of having such an implant in your body will be like, are extremely different things. Especially when it is unknown to the patient what the complete set of consequences of such a device will be. How will the implant feel? What will others see of it? How well will it stay in place? Will it restrict the patient in any way? All questions that are answered differently depending on the patient sitting across from the table. Emphasis on the PPD as part of the medical process at least ‘normalizes’ the effort and makes sure this almost ‘existential therapy’ is part of the routine.
In order to assess the actual level of ‘incorporation’ or ‘existential reorientation’, we suggest the addition of a form of ‘Patient Transparency Diagnosis’ (PTD), with which physicians, engineers and other neuro-engineering experts take the time during the process to together with the patient reflect on how the incorporation is going, and especially, on how to improve this if necessary.
Patient Transparency Diagnosis
Although the previously discussed PPD is already quite incorporated into the medical field, it is important, especially when it comes to neuro-engineering, to look at the whole of the process and assess its success. Most importantly is to realize what to judge this success by. Previously we have discussed the concepts of functionality, sensory feedback and emotional tolerance. However, what we were actually assessing were three concepts that in theory and often in practice lead to transparency and incorporation into the body schema. As one of the patients of Dalibert describes, as it ‘belonging to their body’. Dalibert describes this as follows: “while embodiment of SCS is necessary to live with the technology, it is not sufficient to live well with it: the technology must be incorporated”. (p. 7745) [20].
Therefore, it is important to have regular reflective conversations with patients on the level of transparency and incorporation of their device throughout the neuro-engineering intervention process, as well as afterwards. These conversations will have to center around the actual current level of transparency, the desired level of transparency given the desired level of incorporation, as well as the importance the patient would like to adhere to the concept of transparency in the first place. These questions that will have to be asked to truly assess this, are to their core phenomenological, asking a patient to communicate his or her experience with the device form their perspective, within their situational being-in-the-world. It is here where doctors or engineers are asked to think as phenomenologists, and get to the core of the patient’s experience. Not only will these questions lead to immediate feedback for the medical profession and its success in the field of neuro-engineering, but it will also allow for possible adjustments of the device to the likings of the patient. Imagine a Mrs. Bloemen, who is self-conscious about her husband seeing the device in her back and as such seems to be stuck on the concept of ‘Body Image’ as Merleau-Ponty discusses. Figuring out this underlying problem, and what is the assumption behind it (e.g. ‘I am not truly feminine if I have such a bulge sticking out from by back’) through phenomenological inquiry. This discovery might give opportunities to cater to her wishes, in such a way that Mrs. Bloemen herself was not aware of. Perhaps, next time the battery of the device needs to be changed surgically, the surgeons can decide to place the stimulator on a more subtle location, in line with the preferences of mrs. Bloemen.
For a patient receiving a neuro-engineering device for medical reasons, the body in itself has lost its transparency when it turned into an ‘ill body’. Complete regain of transparency might therefore be difficult or impossible. However, the ultimate goal a device could reach is giving a patient the feeling of ‘belonging somewhere again, as being part of life’ (p.647) [19]. As Slatman herself describes, there is no straightforward, pre-existing mold in which we can pour every neuro-engineering device to reach this ultimate goal. As was clear from our examples, not even the location of implantation, the shape of the device or the workings of the device are easily generalized. For children, different criteria need to be met than for adults. For women, different aspects play a role than for men. And for woman A, different criteria are relevant than for woman B.
The Body as both Leib and Körper
Previously we have discussed how the notion of intentionality makes two different dimensions of the body visible: the body as intentional object or as holding an intentional orientation. Or in other words, ‘having a body’ versus ‘being a body’ [19].
This distinction of the body as a thing and the body as a non-thing, is also described by Husserl using the terms Leib and Körper. On the one hand Husserl distinguishes an animate reality, which is constituted by what he calls Leib. This animate body co-exists with the inanimate matter, which he calls Körper. The co-existing nature is important to emphasize: the two terms refer to different aspects of one and the same living body. According to Husserl it is the Leib which is the medium or organ of all perceptions (Wahrnemungsorgan [19]). This distinction between Leib and Körper is sometimes also described as a distinction between the ‘pre-reflective body-awareness’ on the one hand and ‘reflective consciousness’ on the other hand [34].
As a final practical recommendation, we propose the importance of both patient and doctor to be able to ‘oscillate’ between these concepts of Leib and Körper. The concept of ‘oscillations’ is discussed by Carel et al. in the Lancet [35]:
“Our suggestion is to try to move from viewing the physician’s perspective as objective and the patient’s perspective as subjective towards a greater appreciation of the oscillation from one position to the other. This oscillation does not denote an inconsistency. On the contrary: it marks the unique duality of the human body, which is capable of both subjective experiencing and of being experienced by others as an object. Recognizing the oscillation as key to understanding human experience in its openness and vulnerability might serve as a step towards contesting the expectation that doctors should be purely objective in their clinical practice.” (p.2335) [35]
By allowing the patient and the doctor to oscillate, both separately and as a team, between seeing the body as an object, a machine with a problem to fix using engineering, and the body as lived, as body which needs to incorporate the engineering device as its own in order to be able to function properly, the doctor and patient will cover all relevant grounds of the process. While as we saw, functionality and sensory feedback pushes us towards a more Körper view of the body, it is necessary to progressively move towards promoting and achieving transparency. Once the physical constraints and necessities are addressed, we can focus on the emotional, and affective side of tolerance, the inter-patient difference which is tied to each patient’s being-in-the-world and his wishes, wants and expectations that come with that. The fact that we here seem to speak of oscillation to illustrate the process, however, must not fool us into believing that the concepts of Leib and Körper are any less intertwined than they actually are. It is worth noting that the Leib-aspect of the experience of the body in itself is very much linked to a knowledge of the state of the Körper, continuously making the one an inevitable (counter-)part of the other.
Conclusion
We started out this article by bringing forward the importance of human experience in neuro-engineering endeavors, and the lack of exposure of and practical guidelines on the aspect of tool embodiment in current discussions. In order to bridge this gap, we have zoomed in on some typical case examples, through which we have been able to apply the relevant phenomenological concepts. In addition to elaborating on the general concept of embodiment, in relation to theories on body schema and body image from philosophers such as Merleau-Ponty, we have taken the concepts of functionality, sensory feedback, and affective tolerance as points of reference. After applying these concepts to the field of neuro-engineering in particular, we were able to conclude that indeed the concepts helped to explain and understand patients’ experiences. While not claiming to be conclusive in this aspect, the current paper does draw up a first, broad outline of the concepts at stake when approaching neuro-engineering with a phenomenological outlook.
Next, we have made suggestions for practical implication in which neuro-engineering seems to need and be able to collaborate with phenomenology. We have seen how previously discussed general concepts on tolerance after neuro-engineering interventions will never draw the complete picture for the patient. Indeed, the process involved in neuro-engineering is a very individual and personal one. In the lacuna that is found between adherence to the concepts of functionality, feedback and affective tolerance on the one hand, and the actual success of incorporation of the device by the patient on the other hand, lies a field where neuro-engineering and phenomenology overlap and are ‘on the same team’.
From here on out we have moved on to argue for the introduction of ‘Patient Transparency Diagnosis’ (PTD), which will allow an engineer, doctor or any other relevant expert to use phenomenological inquiry as a way to successfully guide, facilitate and encourage the incorporation of a neuro-engineering device into a patient’s body schema, eventually leading up to a satisfactory level of transparency and existential reorientation.
In addition, we have discussed what practical recommendation and/or guidelines could be extracted from this line of argumentation. Firstly, we have discussed the importance of a ‘Patient Preference Diagnosis’ (PPD), which although more and more recognized in the medical field, deserves more attention as a way to start-off a neuro-engineering endeavor between a patient and his team of experts and warm up the patient for the existential reorientation which will follow from the process. Secondly, additional to the focus on PPD before starting the neuro-engineering process with a patient, a PTD during and after such a process is also relevant when wanting to provide the medical field in general with feedback, and the patient in particular with possibilities to fine-tune the device. Lastly, we have discussed how, by allowing the patient and the doctor to oscillate between the Leib and Körper aspect of the body, we open up opportunity to better reach a state of transparency, and as such, embodiment of neuro-engineering tools.
By emphasizing the role phenomenological considerations can play within the field of neuro-engineering, we not only provide the field in general and the patient in particular with an opportunity to benefit from this perspective, but also show what synergistic collaboration neuro-engineering and phenomenology can establish. To be able to actually achieve this potential benefit of phenomenology, the field of neuro-engineering should not only be aware of phenomenological practice, but should facilitate its application, be it in the form of phenomenological representatives in multidisciplinary teams or embedding of phenomenological approaches in (medical) education to cater for future generations of professionals.
Notes
Throughout this paper, we refer to the users of neuro-engineering devices as ‘patients’, as we are ultimately writing with a clinical perspective in mind. Nevertheless, literature in the field of disability-studies by authors such as Wolbring [4] argues that associating users of a neuro-engineering device with ‘patients’ in general is troubling, as it shows a coverage of disability from a mostly medical angle, emphasizing an assumed experience of a ‘lack in ability’ in these individuals. Instead they argue that while neuro-engineering users might be considered disabled, they can at the same time not understand themselves as ‘patients’, but rather differently abled or just ‘able’. In the context of this paper, however, we continue to use the term ‘patient’ given our medical focus.
The term ‘ownness’ refers to the term as used within the theoretical framework of Edmund Husserl [25]. In the context of the current manuscript, ‘ownness’ is used as describing the delimitation of the self or the ‘ego’ in Husserl’s terms, consisting of everything that is particularly one’s own, in contrast to everything that is alien or ‘Fremdes’, again in Husserlian terms.
One could imagine cases in which transparency is not or not immediately a goal of a neuro-engineering research team, such as in cases asking for ‘quick and dirty’ solutions for life-threatening scenarios. Nevertheless, this manuscript and the current paragraph in particular, argue for reaching transparency in cases where this is possible and wished for based on the idea of incorporation of a device as a part of the ‘normal’ body. This both from the point of view of the research teams involved, as well as and especially from the point of view of the patients, as will be discussed in upcoming sections.
Abbreviations
- ALS:
-
Amyotrophic lateral sclerosis
- BCI:
-
Brain computer interface
- DBS:
-
Deep brain stimulation
- PPD:
-
Patient preference diagnosis
- PTD:
-
Patient transparency diagnosis
- SCI:
-
Spinal cord injury
- SCS:
-
Spinal cord stimulation
References
Vansteensel, Mariska J., Elmar G.M. Pels, Martin G. Bleichner, Mariana P. Branco, Timothy Denison, Zachary V. Freudenburg, Peter Gosselaar, Sacha Leinders, Thomas H. Ottens, Max A. van den Boom, Peter C. van Rijen, Erik J. Aarnoutse, and Nick F. Ramsey. 2016. Fully implanted brain–computer interface in a locked-in patient with ALS. New England Journal of Medicine 375: 2060–2066. https://doi.org/10.1056/NEJMoa1608085.
Capogrosso, Marco, Tomislav Milekovic, David Borton, Fabien Wagner, Eduardo Martin Moraud, Jean-Baptiste Mignardot, Nicolas Buse, Jerome Gandar, Quentin Barraud, David Xing, Elodie Rey, Simone Duis, Yang Jianzhong, Wai Kin D. Ko, Qin Li, Peter Detemple, Tim Denison, Silvestro Micera, Erwan Bezard, Jocelyne Bloch, and Grégoire Courtine. 2016. A brain–spine interface alleviating gait deficits after spinal cord injury in primates. Nature Publishing Group 539: 284–288. https://doi.org/10.1038/nature20118.
Durand, Dominique M. 2007. What is neural engineering? Journal of Neural Engineering 4. https://doi.org/10.1088/1741-2552/4/4/E01.
Wolbring, Gregor, Lucy Diep, Sophya Yumakulov, Natalie Ball, Verlyn Leopatra, and Dean Yergens. 2013. Emerging therapeutic enhancement enabling health technologies and their discourses: What is discussed within the health domain? Healthcare 1: 20–52. https://doi.org/10.3390/healthcare1010020.
Schreuder, Martijn, Angela Riccio, Monica Risetti, Sven Dähne, Andrew Ramsay, John Williamson, Donatella Mattia, and Michael Tangermann. 2013. Artificial intelligence in medicine user-centered design in brain – computer interfaces — A case study. Artificial Intelligence in Medicine 59: 71–80. https://doi.org/10.1016/j.artmed.2013.07.005.
Kübler, Andrea, Elisa M. Holz, Angela Riccio, Claudia Zickler, Tobias Kaufmann, Sonja C. Kleih, Pit Staiger-Sälzer, Lorenzo Desideri, Evert Jan Hoogerwerf, and Donatella Mattia. 2014. The user-centered design as novel perspective for evaluating the usability of BCI-controlled applications. PLoS ONE 9. https://doi.org/10.1371/journal.pone.0112392.
Bod Plass Oude, Danny, Mannes Poel, and Anton Nijholt. 2011. A study in user-centered design and evaluation of mental tasks for BCI. In Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics), 6524 LNCS: 122–134. https://doi.org/10.1007/978-3-642-17829-0_12.
Nijboer, Femke. 2015. Technology transfer of brain-computer interfaces as assistive technology: Barriers and opportunities. Annals of Physical and Rehabilitation Medicine 58: 35–38. https://doi.org/10.1016/j.rehab.2014.11.001.
Burwell, Sasha, Matthew Sample, and Eric Racine. 2017. Ethical aspects of brain computer interfaces: A scoping review. BMC Medical Ethics 18. https://doi.org/10.1186/s12910-017-0220-y.
De Haan, Sanneke, Erik Rietveld, Martin Stokhof, and Damiaan Denys. 2017. Becoming more oneself? Changes in personality following DBS treatment for psychiatric disorders: Experiences of OCD patients and general considerations. PLoS ONE 12. https://doi.org/10.1371/journal.pone.0175748.
Cyron, Donatus. 2016. Mental side effects of deep brain stimulation (DBS) for movement disorders: The futility of denial. Frontiers in Integrative Neuroscience 10. https://doi.org/10.3389/fnint.2016.00017.
Klaming, Laura, and Pim Haselager. 2013. Did my brain implant make me do it? Questions raised by dbs regarding psychological continuity, responsibility for action and mental competence. Neuroethics 6: 527–539. https://doi.org/10.1007/s12152-010-9093-1.
Unterrainer, Marcus, and Fuat S. Oduncu. 2015. The ethics of deep brain stimulation (DBS). Medicine, Health Care and Philosophy 18: 475–485. https://doi.org/10.1007/s11019-015-9622-0.
Jeunet, Camille, Bernard Nkaoua, Sriram Subramanian, Martin Hachet, and Fabien Lotte. 2015. Predicting mental imagery-based BCI performance from personality, cognitive profile and neurophysiological patterns. PLoS ONE 10. https://doi.org/10.1371/journal.pone.0143962.
Lewis, Catharine J., Franziska Maier, Nina Horstkötter, Alicja Zywczok, Karsten Witt, Carsten Eggers, Thomas D. Meyer, T.A. Dembek, M. Maarouf, E. Moro, M. Zurowski, C. Woopen, J. Kuhn, and L. Timmermann. 2015. Subjectively perceived personality and mood changes associated with subthalamic stimulation in patients with Parkinson’s disease. Psychological Medicine 45: 73–85. https://doi.org/10.1017/S0033291714001081.
Heersmink, Richard. 2013. Embodied tools, cognitive tools and brain-computer interfaces. Neuroethics 6: 207–219. https://doi.org/10.1007/s12152-011-9136-2.
Gilbert, Frederic, Mark J. Cook, Terence J. O’Brien, and Judy Illes. 2017. Embodiment and estrangement: Results from first-in-human “intelligent BCI” trial. Science and Engineering Ethics. https://doi.org/10.1007/s11948-017-0001-5.
Clark, Andy. 2013. Re-inventing ourselves: The plasticity of embodiment, sensing, and mind. In The transhumanist reader: classical and contemporary essays on the science, technology, and philosophy of the human future, 113–127. https://doi.org/10.1002/9781118555927.ch11.
Slatman, Jenny. 2014. Our strange body: Philosophical reflections on identity and medical interventions. Amsterdam: University Press.
Dalibert, Lucie. 2016. Living with spinal cord stimulation. Science, Technology & Human Values 41: 635–659. https://doi.org/10.1177/0162243915617833.
Schulte-Mattler, Wilhelm J. 2015. Amyotrophe Lateralsklerose (ALS). Neurophysiologie-Labor 37: 233–239. https://doi.org/10.1016/j.neulab.2015.09.001.
Musarò, Antonio. 2013. Understanding ALS: New therapeutic approaches. FEBS Journal 280: 4315–4322. https://doi.org/10.1111/febs.12087.
Angeli, Claudia A., V. Reggie Edgerton, Yury P. Gerasimenko, and Susan J. Harkema. 2014. Altering spinal cord excitability enables voluntary movements after chronic complete paralysis in humans. Brain 137: 1394–1409. https://doi.org/10.1093/brain/awu038.
Harkema, Susan, Yury Gerasimenko, Jonathan Hodes, Joel Burdick, Claudia Angeli, Yangsheng Chen, Christie Ferreira, et al. 2011. Effect of epidural stimulation of the lumbosacral spinal cord on voluntary movement, standing, and assisted stepping after motor complete paraplegia: A case study. The Lancet 377: 1938–1947. https://doi.org/10.1016/S0140-6736(11)60547-3.
Kockelmans, Joseph J. 1994. Edmund Husserl’s phenomenology. West Lafayette: Purdue University Press.
van Diemen, Tijn, Christel van Leeuwen, Ilse van Nes, Jan Geertzen, and Marcel Post. 2017. Body image in patients with spinal cord injury during inpatient rehabilitation. Archives of Physical Medicine and Rehabilitation 98: 1126–1131. https://doi.org/10.1016/j.apmr.2016.10.015.
Bailey, K. Alysse, Kimberley L. Gammage, Cathy van Ingen, and David S. Ditor. 2017. “My body was my temple”: A narrative revealing body image experiences following treatment of a spinal cord injury. Disability and Rehabilitation 39: 1886–1892. https://doi.org/10.1080/09638288.2016.1211753.
Lawrence, Natalie Kerr. 2008. On social psychology and human nature: An interview with Roy Baumeister. Teaching of Psychology 35: 132–138. https://doi.org/10.1080/00986280802035044.
Aymerich-Franch, Laura, and Gowrishankar Ganesh. 2016. The role of functionality in the body model for self-attribution. Neuroscience Research 104: 31–37. https://doi.org/10.1016/j.neures.2015.11.001.
Lo, Charles, Yvonne Tran, Kim Anderson, Ashley Craig, and James Middleton. 2016. Functional priorities in persons with spinal cord injury: Using discrete choice experiments to determine preferences. Journal of Neurotrauma 33: 1958–1968. https://doi.org/10.1089/neu.2016.4423.
Mittmann, Nicole, Sander L. Hitzig, and B. Catharine Craven. 2014. Predicting health preference in chronic spinal cord injury. The Journal of Spinal Cord Medicine 37: 548–555. https://doi.org/10.1179/2045772314Y.0000000249.
Gallagher, Shaun. 1986. Body image and body schema: A conceptual clarification. Journal of Mind and Behaviour 7: 541–554. https://doi.org/10.2307/43853233.
Godlee, Fiona. 2012. Diagnosing the patient’s preference. BMJ 345: 7745. https://doi.org/10.1136/bmj.e7745.
Gallagher, Shaun. 2014. Phenomenology and embodied cognition. In Routledge handbook of embodied cognition, 9–18. https://doi.org/10.4324/9781315775845.ch1.
Carel, Havi, and Jane MacNaughton. 2012. The art of medicine: “How do you feel?”: Oscillating perspectives in the clinic. The Lancet 379: 2334–2335. https://doi.org/10.1016/S0140-6736(12)61007-1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that there is no conflict of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Tbalvandany, S.S., Harhangi, B.S., Prins, A.W. et al. Embodiment in Neuro-engineering Endeavors: Phenomenological Considerations and Practical Implications. Neuroethics 12, 231–242 (2019). https://doi.org/10.1007/s12152-018-9383-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12152-018-9383-6