Abstract
We explored the care experiences and needs of the home caregivers of patients with amyotrophic lateral sclerosis (ALS) to improve their quality of life. We interviewed home caregivers in-depth and analyzed the data using Colaizzi's descriptive phenomenological method. We interviewed 11 home caregivers of patients with ALS with a disease duration between 1.5 and 4 years. Primary caregivers were predominantly female and were the patients' spouses. Daily caregiving time averaged 4–14 h for 0.5–3.5 years. Interview themes included helplessness and adaptation to life changes, hopelessness, compassion for the patient’s prognosis, and expectation for diverse support. The study sample size was limited, as all participants were from a single tertiary hospital, and all patients had severe functional impairment. Caregivers of patients with ALS experience a considerable burden. Patients and their caregivers can benefit from diversified support channels, and assistive communication systems can be applied to home care. Future research will focus on in-home public long-term care services in China.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Amyotrophic lateral sclerosis (ALS) is a fatal multi-system neurodegenerative disease, which typically manifests as progressive muscle weakness and atrophy [1]. As the disease progresses, patients eventually die from respiratory muscle involvement, paralysis, or concurrent lung infections. The average survival time ranges between 2 and 5 years from symptom onset [2].
Rapid disease progression is associated with an increased demand for care manifestation and rapid progression of ALS. It is crucial to facilitate patient-centered care and incorporate patient perspectives in treatment evaluations [3]. Throughout the progression of ALS, caregivers encounter a multitude of potential stressors, encompassing the ramifications of an unfavorable prognosis, the absence of curative interventions, the physical decline of the patient, alterations in the patient's cognitive or behavioral functioning, and the accumulation of caregiving obligations [4, 5]. These combined stressors, coupled with the intertwined nature of life with the patient, put care partners at risk of heightened burden, psychological distress, and diminished quality of life [6]. Caregivers often struggle with the fact that their loved one has developed a fatal disease and with increased caregiving responsibilities, concerns for the future, and feelings of guilt. As the disease progresses, caregivers of patients with ALS not only experience an increasing amount of physical and mental stress but also substantially increased restrictions on their personal lives and social activities [7]. Quality of life involves understanding an individual's perception of their specific circumstances within the context of their culture, societal values, and place of residence. It also takes into account their personal goals, expectations, standards, and interests [8]. A deeper understanding of the experiences and needs of the home caregivers of patients with ALS is essential to help them improve the quality of life (QoL) of the person they are caring for, as well as to alleviate the caregivers’ concerns and fears about the future.
In China, the primary health care system is inadequate, and filial piety and familial intimacy play a crucial role in patient care; consequently, inexperienced caregivers, namely informal caregivers, such as the patient's children or spouse, often bear all the responsibilities and obligations of care [9]. Informal caregiving is typically characterized by voluntary assistance provided within existing social relationships without financial compensation or specialized training [10]. The progressive nature of ALS requires caregivers to continually adapt to evolving needs [11]. A review of informal caregivers' needs for individuals with ALS indicated that the majority of included articles were from the UK, EU, and Australia, with a smaller number from Turkey, the USA, South Korea, Canada, and Norway. Most studies focused on family caregivers as the primary informal caregivers. These studies identified several common needs across four caregiving stages: post-diagnosis (stage 1), ongoing care (stage 2), end-stage care (stage 3), and bereavement (stage 4). Healthcare professionals should be attentive to the specific caregiving stage to provide appropriate support for informal caregivers [12].
In ALS care, improvement of the quality of life of family members and other caregivers is always necessary to improve the quality of life of the patient himself or herself. For this purpose, it is essential to establish care with the cooperation of multiple professions, home care, and public care services to reduce the burden of care for family members. However, there is currently a dearth of evidence regarding the experiences and needs of informal caregivers in China and limited knowledge regarding their living conditions. To bridge this gap in the existing literature, this article aims to contribute new insights through interviews. Specifically, the article seeks to explore the experiences and needs of informal caregivers of individuals with ALS in China. In this context, needs refer to the abilities of informal caregivers to derive benefit from support.
Materials and Methods
Research Aims and Design
As a phenomenological study, this research adopted a prospective design and collected data through semi-structured, face-to-face in-depth interviews. Before each interview, the research team provided participants with a comprehensive explanation of the purpose and significance of the study, the duration of the interview, potential benefits and risks of participating in the research, and data collection and processing methods. Both patients and primary caregivers were made aware that they could withdraw from the research at any point. This study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of the First Hospital of Shanxi Medical University. Participants agreed to participate in the study voluntarily and provided written informed consent. Confidentiality of the interview responses was maintained. Moreover, all participants’ data were anonymized to protect their privacy, and the collected data were used exclusively for this study.
Research Setting and Participant Characteristics
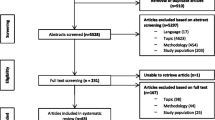
In this study, the primary home caregivers of patients with ALS who were admitted to the neurology department of a tertiary general hospital between June 2019 and January 2020 were recruited as the research participants through purposive sampling. The inclusion criteria were as follows: 1) acting as the primary caregiver of the patient, with total care time ≥ 3 months, or if there were multiple caregivers, providing care for the longest period; 2) age between 18 and 80 years; 3) commitment to no less than 4 h of daily care; 4) no history of other major life events, such as bereavement, unemployment, or divorce, in the previous year; 5) capacity for normal communication and comprehension; and 6) awareness of the purpose of the research and agreement to participate. The exclusion criteria were 1) the use of nannies, care workers, or other paid caregivers and 2) a history of mental illness, severe physical illness, or cognitive impairment. The Amyotrophic Lateral Sclerosis Functional Rating Scale-Revised (ALSFRS-R) was used to assess the functional level of the patients with ALS in 12 items: speech clarity, salivation, swallowing, handwriting, handling utensils, dressing and hygiene, turning in bed and adjusting the bedding, walking, climbing stairs, dyspnea, orthopnea, and the use of assisted mechanical ventilation. Each item was scored on a 5-point scale (0–4 points; total possible score = 48 points). Lower scores indicated severe functional impairment. Disease severity was categorized into mild (37–48 points), moderate (25–36 points), and severe (0–24 points). The Cronbach’s α coefficient for the ALSFRS-R used for assessing ALS in China was 0.88[6]. The patient's quality of life was assessed using the ALSAQ-40 assessment questionnaire, primarily through self-assessment by the patients. This questionnaire covers various aspects of the patient's daily functioning and psychological well-being, including standing, walking, turning over, hand function, eating, dressing, speech and communication, and overall psychological state. It consists of 40 items, each scored from 0 to 4 based on the frequency of occurrence, with 0 indicating no occurrence and 4 indicating a total time. The total score ranges from 0 to 160, with higher scores indicating better daily living abilities and psychological conditions. Previous studies have demonstrated that the Cronbach's α coefficient of this questionnaire falls within the range of 0.90 to 0.96, indicating high internal consistency and reliability [8, 13, 14].
Data Collection
Based on a literature review, an interview outline was developed according to the purpose of the study. The team started with the burden of family care in varying disease progression, trying to fully understand the true feelings of family caregivers and to collect as much information as possible. Before the interview, consent was obtained from the participants, and the interview was conducted when study participants were emotionally stable and willing to communicate. The location of the interview was selected according to the participants’ choice and could be in a quiet office in the hospital or at home. The interview was conducted following the interview outline and recorded using both audio recording and notes, with the notes mainly objectively recording non-verbal behavior such as posture, intonation, and facial expressions of the participants.
Each interview lasted 60–90 min, and during this time, the interviewees were encouraged to fully express their feelings, thoughts, and experiences. At the end of the interview, the participants were asked if there was anything else they needed to add and were thanked for their support and cooperation. The research team began by asking participants about the burden of family care at different stages of the disease to fully understand the true feelings of family caregivers while collecting as much detailed information as possible. The interview outlines were as follows:
-
(1)
When was your loved one (such as a child or parent) diagnosed with ALS? Could you please talk about the disease progression and the process of medical treatment?
-
(2)
Why did you choose home care/hospital treatment?
-
(3)
Could you share your routine care experience?
-
(4)
What was the most difficult problem during the care process? How did you deal with it?
-
(5)
Could you please talk about how you adjusted your mental state since you learned that your loved one was diagnosed with ALS?
-
(6)
Has your loved one been affected by you and had any changes in his/her mindset? How did you deal with your loved one when he/she is emotionally upset?
-
(7)
If your loved one can communicate with others in some way, do you think it will help the patient recover and reduce your caregiving stress?
Data Analysis
The interview recordings were transcribed word by word into documents within 24 h of the interviews. Transcriptions included the contents of the notes, such as the expression, tone of voice, and body movements of the subjects at that time, without making any changes or deletions to ensure the authenticity of the data. Subsequently, Colaizzi’s phenomenological data analysis method was applied [15], including 1) carefully reading all data and gaining an overall impression of the content; 2) extracting important statements related to the research phenomenon; 3) encoding recurrent and meaningful opinions; 4) assembling the coded opinions; 5) generating a detailed and exhaustive description; 6) identifying similar opinions, from which one can then summarize a theme concept; and 7) returning to the subject to verify data authenticity. The research team not only assembled the data but also added their independent understanding and reflection.
Reflexivity and Epoch
During the interview, the interviewer followed the principle of nonintervention or non-evaluation and would only listen to the subjects without making any comments to ensure impartiality. The entire interview was recorded and transcribed within 24 h of the recording to reduce possible errors. The transcription process was completed by a researcher and cross-checked by another member of the research team. Subsequently, during data analysis, the researcher and two other researchers performed statement extraction, content coding, classification and induction, and theme identification, followed by a group discussion to reach an agreement. Once all data were analyzed, results were returned to the participant for verification and confirmation.
Results
None of the enrolled primary caregivers withdrew during the study period. Data saturation was reached with Interviewee 11. The basic demographic characteristics of the primary caregivers and patients are listed in Table 1. In the table, the patients are coded as “N + number,” while the corresponding caregivers are coded as “N + number-1 (or number-2).”
Patients with ALS included in this study had a disease duration between 1.5 and 4 years. According to the ALSAQ-40 scores, patients had a poor quality of life. Their primary caregivers were predominantly female (8/11) and were mainly the spouses of the patient (6/11). The average daily caregiving time and years of care were in the range of 4–14 h and 0.5–3.5 years, respectively, indicating that caring for patients with ALS is a time-consuming and difficult task. In the process of data integration and analysis, 3 subject words and 10 sub-subject words were extracted and encoded 134 times. Through verbatim data analysis, the researcher distilled three themes from the content of the interviews about their caregiving experiences: helplessness and adaptation to life changes, hopelessness and compassion for the patient’s prognosis, and gratitude for and expectations of different sources of support.
Theme 1: Helplessness and Adaptation to Life Changes
Changes in Life Focus
When caring for patients with ALS, their basic physiological needs must be prioritized. Participants’ home care experiences indicated that with disease progression, patients with ALS gradually lost the ability to communicate and to perform activities of daily living (ADL), such as independent eating, toileting, turning over in bed, and dressing. Concurrently, they could not seek timely help through verbal communication, resulting in depression and anxiety. Daily care duties significantly increased the caregivers’ burden. Among the different tasks, the participants noted that the frequency of handling the patients’ oral and respiratory secretions as well as urine and feces was relatively high, and the timeliness of care in this aspect was particularly prominent.
“She needs my help in washing, dressing, cleaning, and eating, which makes her feel useless. She has never laughed once since she has become ill.” (N1-1, patient’s husband)
“He weighs 165 pounds. He needs daily care, even though he is now still mobile. When I help him while he uses the bathroom, his weight is too much for me.” (N2-1, patient’s wife)
“He is now lying in bed, unable to move and unable to speak, because of which I had to take early retirement to take care of him. I have to check on him from time to time, helping him turn over every 2 h, handling his urine and stools, and so on.” (N3-1, patient’s wife)
“She has to be accompanied 24 h every day, and we cannot leave her alone. I need to help her turn over, to pee, poo, and to rub her leg now and then. I am already over 60 years old, and I am barely hanging on ….” (N5-1, patient’s husband)
Feeling Lonely and Helpless
The time-consuming task of caregiving left caregivers feeling like they had lost themselves. Decreased social activity participation and a fear of losing control over their lives made caregivers feel extremely sensitive and anxious. As the patient’s disease progressed and the severity of the illness increased, caregivers reported feeling increasingly lonely and helpless.
“I used to have my hobbies, although my life is gone since he became ill. All my time has been spent looking after him. I suffer from frequent insomnia, am about to collapse, and no longer know the meaning of my life ….” (N2-1, patient’s wife)
Attempting Tasks That They Are Not Good at
Adapting to the changes in life and taking on more responsibilities have become significant challenges for caregivers. In addition, many caregivers mentioned that they had to undertake more tasks, including those they were not familiar with, with male spouses completing more housework and female spouses undertaking repairs and making important decisions.
“She used to take care of all the family business, and I did not have to worry about anything. However, since she fell ill, I had to undertake all the housework, including cooking, washing clothes, and tidying up ….” (N5-1, patient’s husband)
Theme 2: Hopelessness and Compassion for the Patient’s Prognosis
Hopelessness About the Future
Caregivers often use negative words while describing the future. The research team suggested that after learning the patient’s prognosis, disease progression, and survival status, the participants often expressed a sense of hopelessness.
“She needs help now, and she cannot manage to eat without help. Her husband has to go to work to earn money, and he also has to take care of their children. I am old now, and I can just do what I can do, cooking, washing clothes, and cleaning her up. I am unable to imagine what could happen if I died one day. I do not dare to think about the future!” (N6-1, patient’s mother)
“After hearing the doctor saying: ‘There is no cure for this disease, and it is a very rare disease, as the chance of catching it is one in 10 million,’ I felt that there was no hope. When I learned more information from the Internet, I collapsed and cried hard.” (N7-1, patient’s daughter)
“Before he got sick, he was a smiling person with a good personality, and ours was a very happy family. Now, he cannot speak clearly, and he does not talk much. He fears that he is a heavy burden to us, and I fear that he would be lost in his depression. Yet, anyway, I cannot help it. I do not dare to think about the future.” (Crying in her hands) (N8-1, patient’s wife)
Compassion for the Patient
When recalling memories of their experiences, caregivers expressed a mixture of emotions, such as fatigue, helplessness, and sadness. Caregivers mostly felt compassionate about the patients and would compare their condition before and after their illness. Additionally, caregivers would try their best to help the patients fulfill their hobbies and needs, as well as attempt to establish good communication with the patients to help both parties alleviate negative emotions.
“My dad was handsome when he was young. In my mind, he used to be like an ‘idol’ and could do anything. When I saw what he became after he was ill, I felt really sad.” (The participant then choked and started crying) (N3-2, patient’s daughter)
“When the diagnosis was made, my mind went blank. I simply could not accept it, and I went to several other hospitals with the same result. He used to be an expert in mechanical technology and also a fan of music and basketball, although now. I have always wondered why he was so unlucky.” (sighing) (N4-1, patient’s wife)
“My daughter had always been sensible and never had me worried. However, after she fell ill, she could not even speak or move easily and did not want to live anymore. When I saw what she became, I felt so sad but had to hold on simply because of her.” (N6-1, patient’s mother)
Theme 3: Gratitude and Expectation for Diverse Support
Support From Family
The caregiver’s role for a patient with ALS cannot be fulfilled by a single person and often requires the entire family or even several families. During the care process, family members often undertake different roles alongside other familial and social obligations. This care burden not only conflicts with the caregiver’s original role but is also affected by objective factors such as the family environment and income.
“My daughter will often come to help and share some medical expenses. We know it is not easy for her and are satisfied with what she has done.” (N2-1, patient’s wife)
“I stayed with him while he was in hospital, and my younger sister would come over to lend me a hand, which made it a lot easier for me.” (N4-1, patient’s wife)
Among the caregivers, spouses would feel particularly guilty about burdening their children. However, they would still acknowledge the support of family members.
“We only have one child who has his own family. He needs to work during the day and look after the patient during the night, which is exhausting. Meanwhile, the in-laws will help them look after their children without any complaints and will come to help whenever they are free.” (N5-1, patient’s husband)
Support From Peer Patient
Caregivers stated that support from other patients with ALS and their family members was extremely helpful while adapting to the life changes brought about by the disease. During the early stage of the disease, in particular, when patients and their family members face both emotional shock and an increased burden of care, the sharing of information and empathy from peer patients helped them become accustomed to life changes.
“I was introduced to an ALS patient group by our doctor-in-charge and recommended the website created by Dongfang Siyu by peer patients. From these channels, I acquired much reliable and useful information.” (N3-1, patient’s wife)
“Some peer patients introduced me to websites and patient groups dedicated to ALS, from which I learned a lot of valuable information, such as about purchase channels, quality comparisons, and prices of assistive devices needed in daily care (e.g., neck braces, ventilator, tracheal tube, and eye tracker). This information saved us a lot of effort.” (N7-1, patient’s daughter)
Support From Medical Staff
Interview results suggested that most caregivers longed for support from medical staff, and those who received help from medical staff during the care period believed that they were affectionate and caring. However, in the context of communication, family members occasionally complained about the lack of human care and compassion in medical institutions and expected more attention. Additionally, caregivers desired frequent updates and developments on treatment plans, as well as easier access to sufficient medical resources. Treatment is often limited when dealing with patients with ALS; hence, compassion, empathy, and consolation are even more important qualities that healthcare professionals should be equipped with for supporting the expectations and needs of patients and their families.
“Sometimes, the doctor would explain the disease to us. Although we could only understand a little, we would now know something about the disease. The nurses would also encourage us and say that ‘the patient looks a lot more energetic today,’ which would cheer us up and help us remain hopeful.” (N8-1, patient’s wife)
“Last time when my father ran out of medicine, I had to go to a big hospital in the capital city to buy it, although I could not make an appointment with the doctor by any means. I turned to the previous doctor-in-chief, and he helped me out. I felt deeply grateful.” (N9-1, patient’s son)
“You must listen to your doctor in terms of treatment as they are professional. I believe in the doctor’s advice and hope that the medical staff can help relieve the patient’s psychological burden.” (N10-1, patient’s daughter)
Support From the Government
Most interviewees mentioned that expensive medical bills and the lack of supportive social services during treatment significantly increased their burden. Therefore, they hoped the government could improve the insurance system and provide multi-channel support, such as community services and trustees, for patients with motor neuron diseases.
“I still hope that the medical insurance system can cover a larger proportion of the expense. Drugs that are more effective, according to the doctors, are not covered by medical insurance and are quite expensive. Although the doctors mentioned that they were not always going to be effective, I had to give it a try so as not to experience regret.” (N4-1, patient’s wife)
“All my time is dedicated to looking after him, leaving me no chance to work. Without income, we are under significant pressure to live and sincerely hope that the government can help us ….” (N2-1, patient’s wife)
Support From Technology
Caregivers stated that they desired more professional home care devices and were willing to try any treatment methods that could be helpful, even those that were deemed ineffective by doctors. Additionally, they were interested in novel technological products that could facilitate communication between the patient and caregiver; however, in the meanwhile, they were worried that such products could be expensive and unaffordable.
“To solve the problem of speech, other patients recommended that we buy the eye control device. Fortunately, it is not very expensive. It has diverse functions, although I can only handle and apply those easily operated.” (N4-1, patient’s wife)
“It will be great to have a place that is dedicated to looking after patients with ALS. They will be more professional and allow me to have more free time. We are willing to participate in any research that can help find a cure for the disease as early as possible. It will help us all.” (N9-1, patient’s son)
Discussion
Cultural Background That Can Increase the Care Burden
Our study shows that primary caregivers spend most of their time on the patients' ADLs. The progressive nature of the disease results in a deterioration in the patient's conditions, and their clinical manifestations become more complicated to manage. Additionally, patients' decreasing ability to attend to their ADLs results in increased dependency on the caregiver, thereby increasing the caregiver's burden of care. This finding is consistent with the findings of a previous study [16]. Caregivers are required to constantly fulfill the basic physiological needs of patients and to cope with any problems that occur during the caregiving process. Many home caregivers are the patients' spouses and children and are generally inexperienced in providing care to the level required by patients with ALS. Consequently, the caregiver's burden of care also increases when there is a mismatch between the patient's needs and the caregiver's ability to cope. In Eastern cultures, women traditionally bear the primary responsibility for domestic duties, which include caring for their children and parents-in-law. This division of labor is influenced by the underlying Confucian ethical framework [17]. In Chinese culture, filial piety encourages family members to take on the role of caregivers. In this study, spouse caregivers emphasized that marital obligation and a sense of responsibility prompted them to become primary caregivers. Caregivers not only bear the responsibility of caring for patients but also suffer from distress and loneliness. Similarly, sociocultural factors and belief systems that prioritize the family system also significantly influence the provision of care in India. The impact of the illness on the family and the role of the family in caregiving for individuals with ALS are significant [18]. Therefore, they should be provided with multiple channels of support and care to help them appreciate the value of life and to find their self-worth despite these obligations.
Medical Team That Can Provide Professional Services
In both this study and multiple foreign studies [14, 19,20,21,22], caregivers mentioned the difficulty of obtaining relevant care information after the patient was diagnosed with ALS. Consequently, most families had to turn to peer patients and the Internet for direct experiences and information. Additionally, most research participants noted that despite being the primary caregiver, they still longed for support from other family members, relatives, peer patients, and professional medical staff. Doctors who provided relevant knowledge, skills, and aids beyond mere medical information were deemed more caring and compassionate. Some caregivers were forced to deal with different problems instantly without any support post-diagnosis. Foreign scholars recommended that the diagnosis of ALS should be staged at a comfortable pace, allowing patients and caregivers to gradually deepen their understanding of the disease as it progresses. It would also give healthcare professionals more time to understand the patient's problems, the status of the family, and social support. Additionally, patients should be informed of their disease progression and given an estimate of their survival; however, help should also be provided to assist them with formulating a living will [23]. By doing so, patients can fulfill their roles and identities in advance and cope with ever-changing family dynamics, thereby preventing them from feeling like a burden to their relatives.
Therefore, strengthening the role of medical staff in supporting the home care of patients with ALS and extending professional healthcare services to the patient's family is crucial. For instance, following a patient's diagnosis, it is imperative to offer scientific and systematic nursing guidance throughout various phases of the illness. This guidance should encompass various aspects, such as the patient's personal factors, including their ability to cope with the diagnosis, the potential reduction in life expectancy, the imminent development of disabilities, and their reliance on others. Additionally, recommendations regarding the anticipation of fistula and ventilator treatment, timely suggestions for assistive devices, empathy towards the patient's emotional fluctuations, and counsel on sustaining a functional and healthy lifestyle should be provided.
Government Support That Can Improve the Medical Insurance System
Our results show that both patients with ALS and their families had a strong desire for medical insurance policy support and improved social security systems. Reliable healthcare insurance systems and higher income levels in developed countries or regions have been associated with lower care burdens [24]. In Korea, for instance, ALS patients are responsible for 44.8% of direct medical costs, while the government covers the remaining expenses [25]. However, in most areas in China, the community treatment of ALS is not included in the scope of medical insurance subsidies. When a family member is diagnosed with a severe illness that requires substantial financial resources, the entire family must contribute to covering the medical expenses, often depleting their savings. As a result, Chinese patients face a heavier financial burden compared to those living in countries with more comprehensive healthcare insurance systems. Additionally, some countries have gradually introduced an evidence-based palliative care model with multidisciplinary cooperation for patients with ALS [26] and have successfully reduced the burden on caregivers by implementing a comprehensive social support system.
To address this, attempts should be made to establish a more comprehensive medical insurance system, which can effectively alleviate the financial burden of caregivers by including some out-of-pocket ALS drugs into the medical insurance subsidy. Concurrently, the primary healthcare system should be improved to provide high-quality and effective nursing services for home caregivers. Moreover, support systems for the caregivers of patients with ALS, such as subsidy policies and vacation systems, should be introduced to alleviate their physical and mental burden and to improve the QoL of both patients and their caregivers.
Technological Applications That Can Improve Quality of Life
Communication barriers increase the difficulty of home care. With disease progression, almost all patients with ALS experience impaired speech, thereby compromising daily communication, which was reflected in our interviews. Communication barriers not only reduce the QoL of both patients and their caregivers but also cause significant difficulties in home care. In interviews, caregivers often expressed their willingness to actively try assistive communication devices that improved their communication with the patient and acknowledged the active role of these devices in daily care. A randomized controlled study [19] found that the mental health of patients with ALS could be enhanced by allowing them to fully express their negative emotions. Multiple studies have shown that the QoL of patients who use assistive communication devices is better than that of patients who do not use them [27]. Thus, the implementation of augmentative and alternative communication interventions is beneficial to both patients and their caregivers, and the application of this communication technology in the home care of patients with ALS should be actively explored. The design of such products should fully consider the progression of ALS, the basic care needs of patients, and the comprehension, competence, and compliance of caregivers such that it can enable communication between the patient and caregiver, improve their physical and psychological experience, and enhance their QoL.
Limitations
This study has some limitations. First, the sample size of the study was limited as all participants were recruited from a single tertiary hospital in Shanxi province, China. Second, the ALSFRS-R score of the patients selected in this study ranged from 0 to 24, indicating severe functional impairment.
Application
In this study, three themes were extracted regarding the experiences of caregivers of patients with ALS: helplessness and adaptation to life changes, hopelessness and compassion for the patient's prognosis, and gratitude for and expectations of different sources of support. The results indicated that home caregivers experienced significant changes in their life focus and were required to constantly satisfy the patient's basic physiological needs, particularly when dealing with the patient’s bodily excretions on time. The heavy burden of care and lack of social interaction made the caregivers feel lonely and helpless. Additionally, communication barriers between the patient and caregiver further increased the difficulties. Our study found that caregivers showed a positive attitude towards technological applications, such as augmentative and alternative communication, and tried their best to help the patients engage in their former hobbies. They also desired a better communication channel with the patient to help reduce the negative emotions felt between them and to effectively alleviate the burden of care. One solution is to actively explore the application of high-tech augmentative and alternative communication in the home care of these patients. Such products should be designed to serve as a communication channel between the patient and caregiver to enhance their QoL. Future studies should be conducted using a larger sample size for a more in-depth analysis. Cases from socioeconomically developed regions of central and eastern China and the less socioeconomically developed regions of western China could be investigated. Ongoing engagement with the caregivers of patients with ALS with different functional levels is essential for improving our understanding of their care experience and needs. Future work should also focus on this direction of research.
Data Availability
Confidentiality of the interview responses was maintained. Moreover, all participants’ personal data were anonymized to protect their privacy, and the collected data were used exclusively for this study.
References
Hardiman, O., et al. 2017. Amyotrophic lateral sclerosis. Nature Reviews Disease Primers 3: 17071.
Masrori, P., and P. Van Damme. 2020. Amyotrophic lateral sclerosis: A clinical review. European Journal of Neurology 27 (10): 1918–1929.
Hogden, A. 2014. Optimizing patient autonomy in amyotrophic lateral sclerosis: Inclusive decision-making in multidisciplinary care. Neurodegenerative Disease Management 4 (1): 1–3.
Anderson, N.H., et al. 2019. “A monster that lives in our lives”: Experiences of caregivers of people with motor neuron disease and identifying avenues for support. BMJ Supportive & Palliative Care 9 (4): e27.
Goldstein, L.H., and S. Abrahams. 2013. Changes in cognition and behaviour in amyotrophic lateral sclerosis: Nature of impairment and implications for assessment. Lancet Neurology 12 (4): 368–380.
Vandepitte, S., et al. 2016. Effectiveness of respite care in supporting informal caregivers of persons with dementia: A systematic review. International Journal of Geriatric Psychiatry 31 (12): 1277–1288.
Ryan, M., et al. 2019. Lifetime Risk and Heritability of Amyotrophic Lateral Sclerosis. JAMA Neurology 76 (11): 1367–1374.
Pavan, K., et al. 2010. Validation of the Amyotrophic Lateral Sclerosis Assessment Questionnaire (ALSAQ-40) scale in the Portuguese language. Arquivos de Neuro-Psiquiatria 68 (1): 48–51.
Qiu, X., J.W.H. Sit, and F.K. Koo. 2018. The influence of Chinese culture on family caregivers of stroke survivors: A qualitative study. Journal of Clinical Nursing 27 (1–2): e309–e319.
Hoefman, R.J., J. van Exel, and W. Brouwer. 2013. How to include informal care in economic evaluations. PharmacoEconomics 31 (12): 1105–1119.
Galvin, M., et al. 2018. Needs of informal caregivers across the caregiving course in amyotrophic lateral sclerosis: A qualitative analysis. British Medical Journal Open 8 (1): e018721.
Poppe, C., et al. 2020. Differentiating needs of informal caregivers of individuals with ALS across the caregiving course: A systematic review. Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration 21 (7–8): 519–541.
Alankaya, N., et al. 2019. Validity and Reliability of the Turkish Version of the Amyotrophic Lateral Sclerosis Assessment Questionnaire. Journal of Neuroscience Nursing 51 (5): 253–258.
Maessen, M., et al. 2007. Validity of the Dutch version of the Amyotrophic Lateral Sclerosis Assessment Questionnaire, ALSAQ-40, ALSAQ-5. Amyotrophic Lateral Sclerosis 8 (2): 96–100.
Lu, Y.F., and J.E. Haase. 2009. Experience and perspectives of caregivers of spouse with mild cognitive impairment. Current Alzheimer Research 6 (4): 384–391.
Galvin, M., et al. 2016. Caregiving in ALS - a mixed methods approach to the study of Burden. BMC Palliative Care 15 (1): 81.
Koh, E.K., and C.K. Koh. 2008. Caring for older adults: The parables in Confucian texts. Nursing Science Quarterly 21 (4): 365–368.
Thomas, P.T., et al. 2018. Caregiver burden and quality of life of patients with amyotrophic lateral sclerosis in India. Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration 19 (7–8): 606–610.
Gordon, P.H. 2013. Amyotrophic Lateral Sclerosis: An update for 2013 Clinical Features, Pathophysiology, Management and Therapeutic Trials. Aging and Disease 4 (5): 295–310.
Lillo, P., E. Mioshi, and J.R. Hodges. 2012. Caregiver burden in amyotrophic lateral sclerosis is more dependent on patients’ behavioral changes than physical disability: A comparative study. BMC Neurology 12: 156.
Pagnini, F. 2013. Psychological wellbeing and quality of life in amyotrophic lateral sclerosis: A review. International Journal of Psychology 48 (3): 194–205.
Cipolletta, S., and L. Amicucci. 2015. The family experience of living with a person with amyotrophic lateral sclerosis: A qualitative study. International Journal of Psychology 50 (4): 288–294.
Burchardi, N., et al. 2005. Discussing living wills. A qualitative study of a German sample of neurologists and ALS patients. Journal of the Neurological Sciences 237 (1–2): 67–74.
Qutub, K., et al. 2014. Life factors affecting depression and burden in amyotrophic lateral sclerosis caregivers. Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration 15 (3–4): 292–297.
Oh, J., et al. 2015. Socioeconomic costs of amyotrophic lateral sclerosis according to staging system. Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration 16 (3–4): 202–208.
MacDermott, C.N., et al. 2017. Review of “Palliative care in Amyotrophic Lateral Sclerosis from diagnosis to bereavement” by David Oliver, Gian Domenico Borasio, Wendy Johnson. BMJ Supportive & Palliative Care 7 (1): 5–6.
Linse, K., et al. 2018. Communication Matters-Pitfalls and Promise of Hightech Communication Devices in Palliative Care of Severely Physically Disabled Patients With Amyotrophic Lateral Sclerosis. Frontiers in Neurology 9: 603.
Acknowledgements
In this section, you can acknowledge any support given which is not covered by the author contribution or funding sections. This may include administrative and technical support, or donations in kind (e.g., materials used for experiments).
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Kun Yang, Hongxia Xue, Li Li. The first draft of the manuscript was written by Kun Yang. The review and editing draft of the manuscript was written by Shan Tang and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of the First Hospital of Shanxi Medical University (Ethics Approval No. [2020] IRB [K076]).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, K., Xue, H., Li, L. et al. Caregivers of ALS Patients: Their Experiences and Needs. Neuroethics 17, 4 (2024). https://doi.org/10.1007/s12152-023-09537-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12152-023-09537-y